New research by University of Georgia scientists sheds light on why people with obstructive sleep apnea may have associated autoimmune disorders. The results could lead to better approaches to treatment and possibly new drug therapies.
The study, led by Bradley Phillips, builds on previous research showing that obstructive sleep apnea increases the risk for autoimmune diseases. Immune system disorders are a result of either low activity or over activity of the immune system and include well known conditions such as lupus and rheumatoid arthritis.
“This paper looks at what may be the underlying mechanisms that increase someone’s risk for autoimmune disorders because they have untreated obstructive sleep apnea,” said Phillips, director of UGA’s Biomedical and Health Sciences Institute.
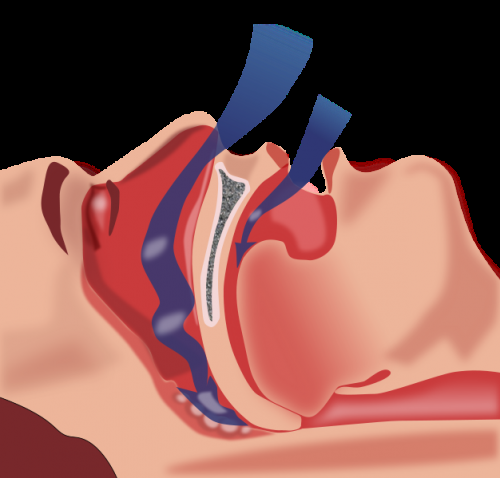
Obstructive sleep apnea, or OSA, is a disorder that occurs when throat muscles relax temporarily, narrowing or collapsing the airway and momentarily cutting off breathing during sleep. The main treatment for OSA is continuous positive airway pressure, or CPAP, which pumps air through a mask to keep the airway open. About 40% of patients can’t tolerate CPAP.
OSA damages the health of 35% of Americans and results in increased risk of several autoimmune disorders, like rheumatoid arthritis and psoriasis, for example, but the molecular links to autoimmunity are poorly understood.
Phillips and the team looked at four cytokines—proteins involved in cell signaling—associated with autoimmune disease. They evaluated the cytokines in three groups of adults: patients with untreated OSA, patients with OSA who were receiving treatment, and people who did not have OSA. The study results revealed abnormal levels of the four cytokines in patients with untreated sleep apnea, suggesting that poor sleep and inadequate oxygen supply may affect the cytokines.
This study, published in Clinical Immunology, is one of four investigating possible links between obstructive sleep apnea and specific diseases. In addition to autoimmune disorders, the team is also looking at neurodegenerative disorders, cardiovascular disease and renal disease.
Source: Read Full Article
