The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus that causes the coronavirus disease (COVID-19), causes a wide range of symptoms beyond the respiratory tract.
Many patients report many symptoms impacting the cardiovascular system and the nervous system. There is growing evidence that SARS-CoV-2 infection can include long-term neuropsychological deficits, even in its mild or moderate respiratory forms.
A team of researchers at the Clinical and Experimental Neuropsychology Laboratory, Faculty of Psychology, the University of Geneva in Switzerland, reports that SARS-CoV-2 may affect the central nervous system, particularly the limbic system responsible for behavioral and emotional responses.
The study, published in the pre-print server medRxiv*, demonstrates the presence of long-lasting neuropsychological sequelae after COVID-19, regardless of the respiratory disease's severity.
.jpg)
Study background
Health experts have suspected the presence of long-term neuropsychological deficits after SARS-C0V-2 infection. For instance, previous studies about the two previous coronavirus outbreaks, the severe acute respiratory syndrome (SARS) and the Middle East respiratory syndrome (MERS), demonstrated the presence of neuropsychological symptoms like sleep disorders, emotional lability, impaired concentration, frequent recall of traumatic experiences, impaired memory, and fatigue in more than 15 percent of affected patients about one month to 3.5 years following infection.
Further, in other diseases like the Human Immunodeficiency Virus (HIV), encephalitis, and multiple sclerosis, studies have shown specific long-term deficits in cognitive functions, including emotional responses and memory,
In COVID-19, however, there are reports of increased prevalence of stroke in patients, leading to additional short-and long-term neurological and cognitive deficits. Lastly, the sudden onset of anosmia or the loss of smell has been described as a symptom in COVID-19 patients.
This symptom happens because olfactory epithelium carries angiotensin-converting enzyme 2 (ACE2) receptors, the cellular gateway the virus uses to enter human cells. Scientists formulated that the virus may have used the nose-brain barrier for viral entry.
The study
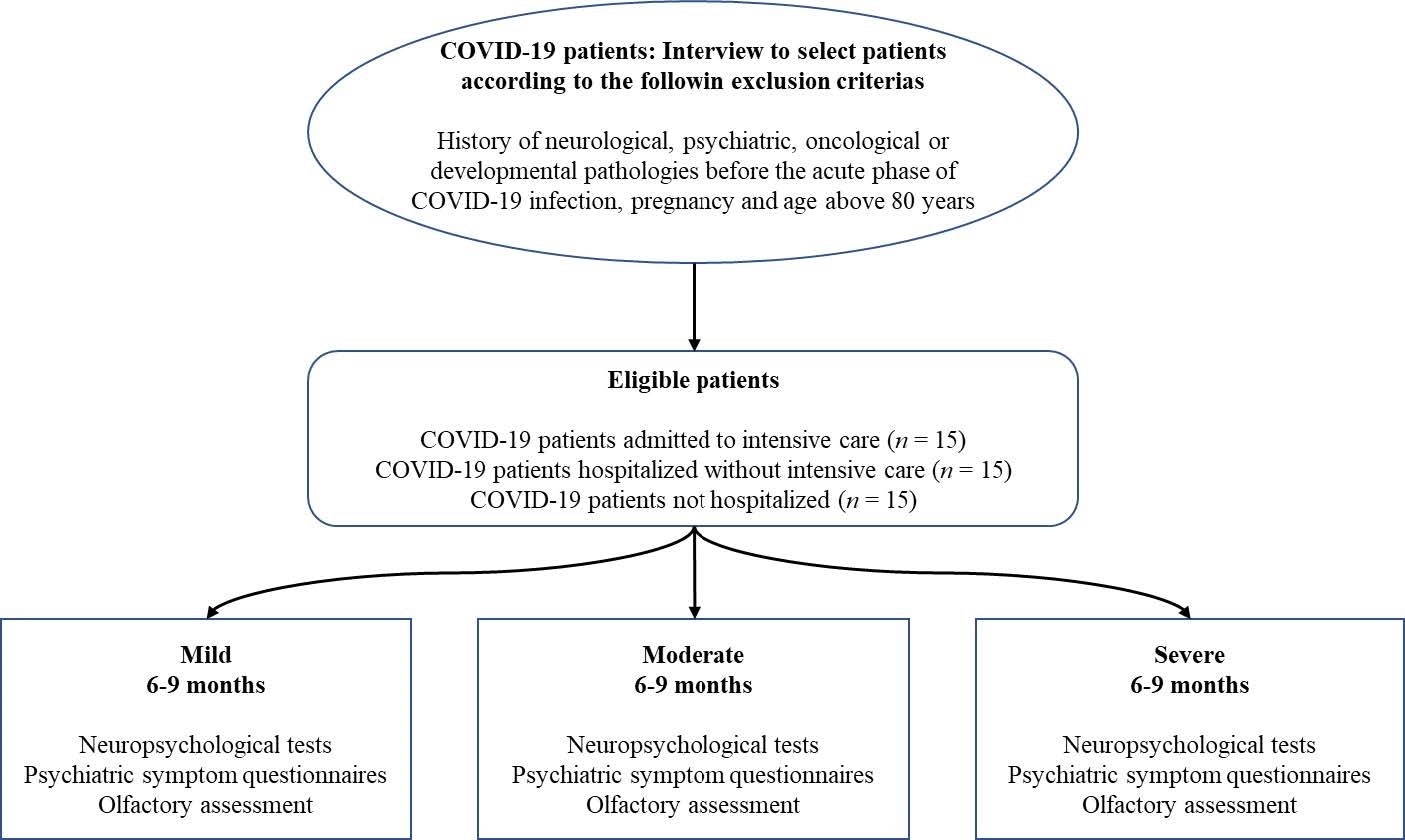
The current study aims to determine the effect of SARS-CoV-2 infection on the brain. The team wants to investigate whether COVID-19 causes long-term neuropsychological deficits from 6 to 9 months, identify the nature of the affected domains, and know the impact of these deficits on the patient's quality of life.
The team administered standardized neuropsychological, neurological, psychiatric, and olfactory tests to 45 patients to arrive at the study findings.
The team divided the patients into three groups, according to the severity of the respiratory disease in the acute phase: severe, moderate, or mild. Severe cases were admitted in the intensive care unit with respiratory assistance, moderate cases were hospitalized without respiratory aid, and mild patients were not admitted to the hospital.
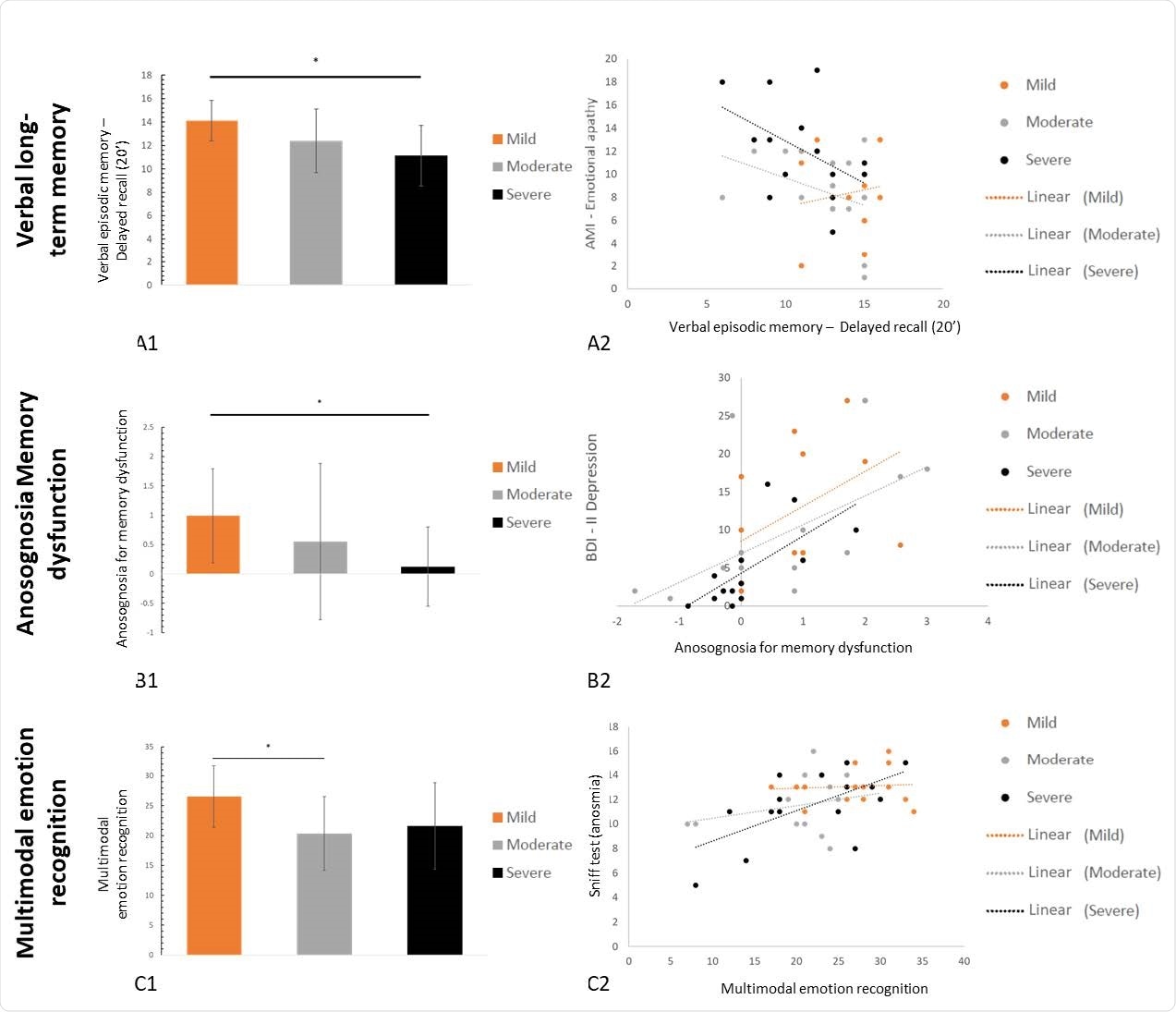
The researchers found a high prevalence of psychiatric symptoms, regardless of disease severity, in the illness's acute phase. Patients in all three groups manifested depressive symptoms, mania, anxiety, stress, apathy, post-traumatic stress disorder (PTSD), and dissociative disorders. Some patients reported insomnia, fatigue, and pathological somnolence.
When it comes to the sense of smell, 33.33 percent of the mild group, 73.33 percent of the moderate group, and 46.66 percent of the severe group have hyposmia or the partial loss of smell six to nine months after being infected. Meanwhile, of the severe group, 13.33 percent still had anosmia or the complete loss of smell.
Though the cognitive deficits reported in the three groups were common, some domains of cognition and mood were impacted differently, depending on the disease's severity. In long-term episodic memory, the severe group patients performed more poorly than the mild group. They also showed more anosognosia for memory dysfunction.
Meanwhile, the mild group was more stressed, anxious, depressed, and reported more cognitive issues. The moderate group recognized multimodal emotions less well than the mild group. All of these manifestations have impacted the patients' lives.
"At this stage, it is difficult to determine whether the cognitive deficits can be regarded as a marker of brain damage and/or should be linked to psychiatric variables that may themselves result directly from infection with SARS-CoV-2 or else be triggered by the stressful nature of the general pandemic and the individual experience of the disease," the researchers explained.
The team recommends that clinical guidelines and recommendations should be implemented in the management of long-term neurological impairment after SARS-CoV-2 infection
*Important Notice
medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Long COVID neuropsychological deficits after severe, moderate or mild infection, P. Voruz, G. Allali, L. Benzakour, A. Nuber-Champier, M. Thomasson, I. Jacot, J. Pierce, P. Lalive, K-O. Lövblad, O. Braillard, M. Coen, J. Serratrice, J. Pugin, R. Ptak, I. Guessous, B.N. Landis, F. Assal, J.A. Péron, medRxiv, 2021.02.24.21252329; doi: https://doi.org/10.1101/2021.02.24.21252329, https://www.medrxiv.org/content/10.1101/2021.02.24.21252329v1
Posted in: Medical Research News | Disease/Infection News
Tags: ACE2, Angiotensin, Angiotensin-Converting Enzyme 2, Anosmia, Anxiety, Brain, Central Nervous System, Coronavirus, Coronavirus Disease COVID-19, Encephalitis, Enzyme, Fatigue, HIV, Hospital, Immunodeficiency, Insomnia, Intensive Care, Laboratory, Limbic System, Mania, Multiple Sclerosis, Nervous System, Pandemic, Post-Traumatic Stress Disorder, Psychology, Respiratory, Respiratory Disease, SARS, SARS-CoV-2, Sclerosis, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Sleep, Stress, Stroke, Syndrome, Virus

Written by
Angela Betsaida B. Laguipo
Angela is a nurse by profession and a writer by heart. She graduated with honors (Cum Laude) for her Bachelor of Nursing degree at the University of Baguio, Philippines. She is currently completing her Master's Degree where she specialized in Maternal and Child Nursing and worked as a clinical instructor and educator in the School of Nursing at the University of Baguio.
Source: Read Full Article
