Taking omega-3 fatty acids and vitamin D3 supplements does not neither increase nor decrease the risk of developing atrial fibrillation, according to late-breaking research presented today at the American Heart Association’s Scientific Sessions 2020.
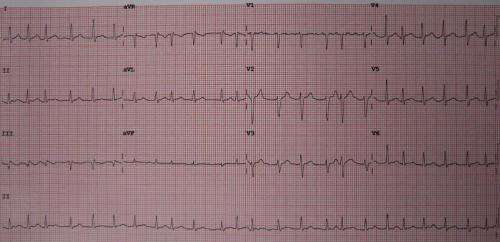
Atrial fibrillation is a rapid, irregular heartbeat caused by chaotic electrical signals in the top chambers of the heart. Atrial fibrillation is the most common heart rhythm disturbance, and it can lead to blood clots, strokes, heart failure and other heart-related complications. Atrial fibrillation risk increases with age, high blood pressure and heavy drinking and can be common among multiple, biologically related family members.
Evidence from previous observational studies has been conflicting, suggesting both risks and potential health benefits of fish oil—a source of omega-3 fatty acids—and vitamin D for atrial fibrillation.
“Once established, atrial fibrillation is difficult to treat and results in symptoms that can impair patients’ quality of life,” said Christine M. Albert, M.D., M.P.H., founding chair of the department of cardiology in the Smidt Heart Institute at Cedars-Sinai Medical Center in Los Angeles and lead author of this study. “Current treatment options have limited long-term success and significant risks, and there is a pressing need for preventive strategies.”
The VITAL Rhythm Trial is the first, placebo-controlled, randomized clinical trial investigating preventive therapies for atrial fibrillation. This trial evaluated whether supplementation with vitamin D3 (2000 IU/day) and omega-3 fatty acids (EPA:DHA in 1.2:1 ratio; 840mg/day) can reduce the risk of developing atrial fibrillation compared to placebo.
The five-year study, from 2012—2017, included 25,119 adults, ages 50 and older who had no history of atrial fibrillation. About half of the participants were female, 21% were black, and the average age was 67. Atrial fibrillation diagnoses were established both by participant self-report and claims data from the Centers for Medicare and Medicaid Services. Electrocardiogram evidence and/or a physician’s report documenting a new diagnosis of atrial fibrillation were required for confirmation.
During the trial follow-up period, 900 participants developed atrial fibrillation, 3.6% of the study population. There were no statistically significant differences between the groups who were assigned to supplemental EPA/DHA and/or vitamin D3 compared to individuals who were assigned to the placebo.
Source: Read Full Article
