Severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) is the causative agent of the ongoing coronavirus disease 19 (COVID-19) pandemic. This pandemic has resulted in drastic healthcare and economic crises, as scientists across the globe are working extensively to develop means to contain the pandemic. Several COVID-19 vaccines have received emergency use authorization (EUA), and in many parts of the world, vaccination programs have commenced.
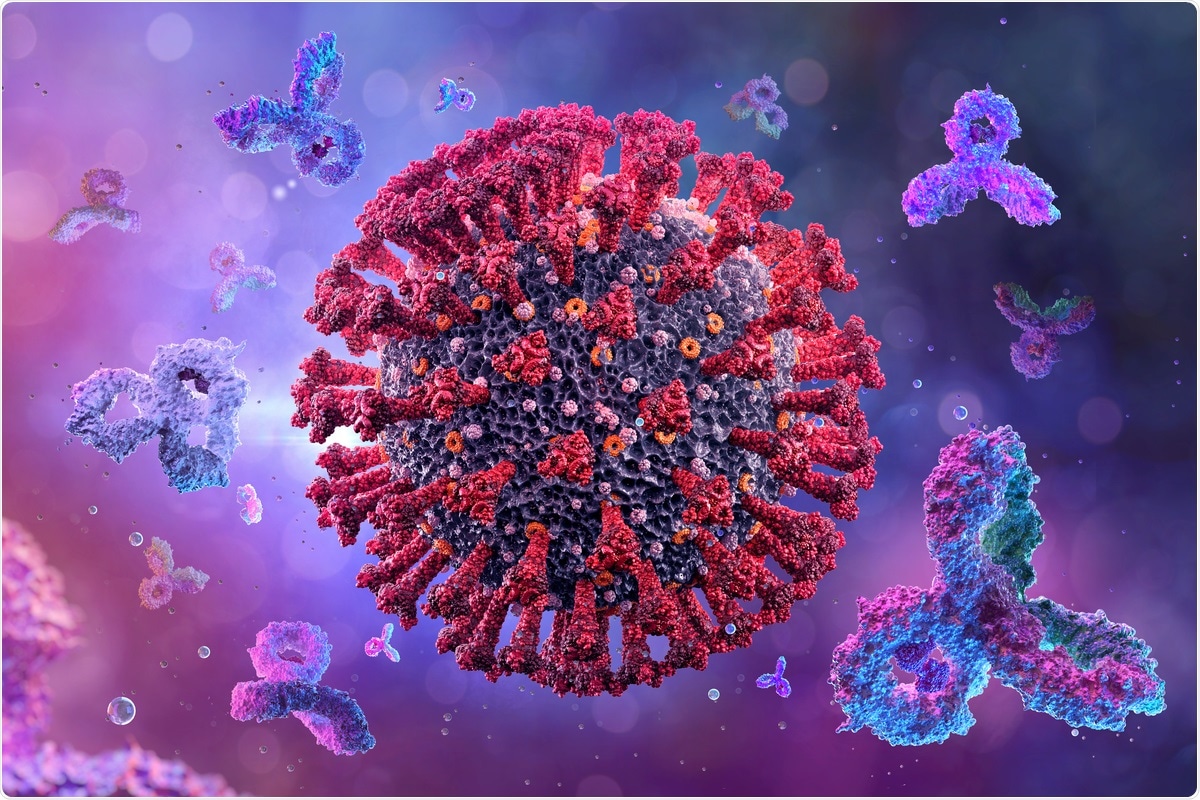 Study: Humoral and cellular immune responses upon SARS-CoV-2 vaccines in patients with anti-CD20 therapies: A systematic review and meta-analysis of 1342 patients. Image Credit: Corona Borealis Studio/ Shutterstock
Study: Humoral and cellular immune responses upon SARS-CoV-2 vaccines in patients with anti-CD20 therapies: A systematic review and meta-analysis of 1342 patients. Image Credit: Corona Borealis Studio/ Shutterstock
Background
Although COVID-19 vaccines protect all individuals across all age groups, immunocompromised patients are still at a high risk of severe infection despite immunization. According to pre-pandemic studies, patients undergoing B-cell depleting therapy are more likely to experience reduced vaccination responses. Additionally, patient factors and disease entities, for example, disease-specific B-cell repopulation kinetics, also influences the degree of immune response rates.
Previous studies associated with the immune response rates post influenza vaccination indicated that an adequate period between anti-CD20 therapy and vaccination is essential. As the global COVID-19 vaccination program is progressing worldwide, at a differential pace in accordance with availability, scientists have focused on better understanding and improving the immunogenicity of vaccines for patients subjected to anti-CD20 therapy.
A new study
A new systematic review and meta-analysis, published on the medRxiv* preprint server, focused on the humoral and cell-mediated immune responses after COVID-19 vaccination in patients undergoing anti-CD20 antibodies treatment. This study aimed to analyze the diseases entities, quantitative measures, and effective duration since the last anti-CD20 therapy.
Scientists reviewed research articles available in EMBASE, SSRN, medRxiv, and PubMed up to August 21st, 2021. They excluded studies that did not meet some specific criteria, such as (a) missing data on humoral or cell-mediated immune responses, b) unspecified methodology of response testing, (c) small sample size, i.e., ≤ three patients, (d) unspecified timeframes between vaccination and blood sampling (e) individual patients with prior SARS-CoV-2 infection, or (f) patients with incomplete vaccine courses. After the screening, the study included a total of 23 articles comprising data from 1342 participants.
The main findings
The study provides overall seroconversion rates and cell-mediated immune responses after SARS-CoV-2 vaccination in patients with a history of anti-CD20 therapies. According to the authors, this is the first published systematic study that focuses on the impact of COVID-19 vaccination in patients undergoing anti-CD20 therapies. This review indicates the existence of significant heterogeneity in the immunogenicity of COVID-19 vaccines, which is partially due to differences in treatment indications.
The review highlighted that the time since the last anti-CD20 therapy administration plays an important role in seroconversion rates. A similar observation had been reported in the context of influenza seroconversion in patients receiving anti-CD20 therapies. Previous reports from the same group of researchers suggested that substantial SARS-CoV-2 vaccine-induced seroconversion rates could occur in patients with a high level of CD4-positive T cell count even when they received anti-CD20 therapy.
Also, the different assays, such as quantitative IGRA and semi-quantitative EliSpot analysis, used in studies related to cell-mediated immunity can drive heterogeneous results. Researchers highlighted that EliSpot was found to be more sensitive for diagnosing tuberculosis than quantitative IGRA.
This study reported the overall rate of humoral response was 0.41, and that of cell-mediated immune response was 0.71. Scientists found a strong association between longer time intervals, between the last anti-CD20 therapy and vaccination, and increased humoral response. They reported higher humoral response rates (0.63) at the time frame of more than six months and lowered humoral response rates of 0.2 at a timeframe below six months, between the last anti-CD20 therapy and COVID-19 vaccination.
This study revealed that kidney transplant patients treated with anti-CD20 therapy showed lower vaccination response rates than hematological malignancies or autoimmune diseases.
Conclusion
Researchers stated that some of the studies included in this review had some limitations. For instance, some participants experiencing asymptomatic COVID-19 were not confirmed via the serological approach, e.g., anti-nucleocapsid immunoassays. Another limitation includes the seroconversion system, whose outcomes are heterogeneous owing to manufacturer cut-offs. This is because of a lack of standardized threshold values to determine protective antibody levels. The authors also stated that sufficient data were not available to evaluate closer discrimination of different autoimmune diseases. Further, researchers did not consult external experts in the field, and clinical study registry data were assessed.
Scientists concluded that patients subjected to anti-CD20 therapies must be vaccinated against SARS-CoV-2. This is based on previous studies documenting successful induction of humoral (41%) and cell-mediated (71%) immune responses, via COVID-19 vaccines, in patients with a history of anti-CD20 therapies.
*Important Notice
medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Schietzel, S. et al. (2021) "Humoral and cellular immune responses upon SARS-CoV-2 vaccines in patients with anti-CD20 therapies: A systematic review and meta-analysis of 1342 patients". medRxiv. doi: 10.1101/2021.09.30.21264335.
Posted in: Medical Science News | Medical Research News | Disease/Infection News
Tags: Antibodies, Antibody, Blood, CD4, Cell, Coronavirus, Coronavirus Disease COVID-19, Healthcare, Immune Response, immunity, Immunization, Immunoassays, Influenza, Kidney, Kidney Transplant, Pandemic, Research, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Syndrome, Transplant, Tuberculosis, Vaccine

Written by
Dr. Priyom Bose
Priyom holds a Ph.D. in Plant Biology and Biotechnology from the University of Madras, India. She is an active researcher and an experienced science writer. Priyom has also co-authored several original research articles that have been published in reputed peer-reviewed journals. She is also an avid reader and an amateur photographer.
Source: Read Full Article
