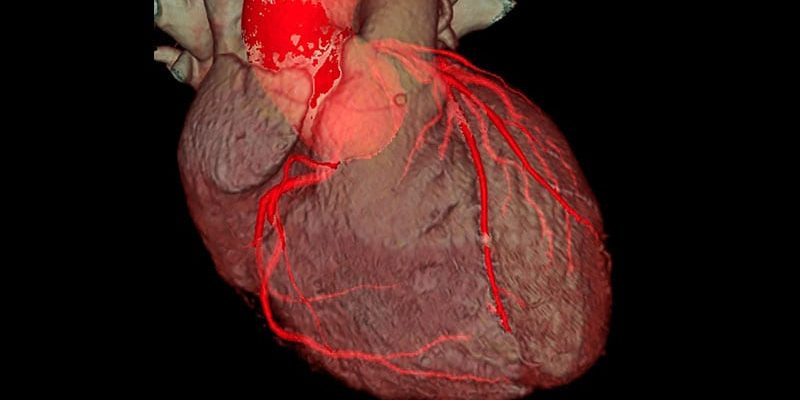
A study of whether use of noninvasive coronary CT angiography (CCTA) can cut down on the use of invasive coronary angiography when making treatment decisions in patients who have undergone previous coronary artery bypass surgery (CABG) has shown mixed interim results.
The GREECE trial was aiming to show that doses of contrast and radiation were lower for the patients who received CCTA before invasive angiography, but the study showed that doses were actually higher in the combination imaging group. But this did not affect the main safety endpoint ― contrast-induced nephropathy ― for which rates were comparable between the two arms. In addition, the procedure time was significantly shorter in the combination imaging group.
The interim results of the GREECE study were presented by Grigorios Tsigkas, MD, from Patras University Hospital, Greece, at the Congress of the European Association of Percutaneous Coronary Interventions (EuroPCR) 2022, being held this week in Paris.
Tsigkas explained to theheart.org | Medscape Cardiology that patients who have undergone CABG surgery have complex anatomy, so further diagnostic imaging with invasive coronary angiography can lead to more fluoroscopy time and higher contrast dose.
Taking into account the high diagnostic accuracy of the noninvasive CCTA in detecting or excluding stenosis or occlusion of CABG grafts, the researchers hypothesized that use of CCTA to assess the grafts could reduce the procedure time needed for invasive coronary angiography and reduce fluoroscopy time and periprocedural complications.
Tsigkas explained that, at present, CCTA does not provide adequate diagnostic accuracy for native coronary arteries, so invasive coronary angiography would still be required for evaluation of these arteries.
“The general thought is that invasive coronary angiography would be useful in native coronary arteries evaluation, while CCTA would be better for graft assessment, and using the combination should cut down exposure to the invasive procedure,” he said.
The GREECE trial was conducted to investigate this question. The study included hemodynamically stable patients who had a previous medical history of CABG and an indication for coronary angiography. Patients were randomly assigned to receive either invasive coronary angiography (control group) or CCTA followed by invasive coronary angiography (intervention group).
Tsigkas presented results from the first 153 patients, which was about half of the planned enrollment.
The primary endpoint ― total volume of contrast agent administered ― was not reduced in the combination arm. In fact, the combination arm received significantly more contrast than the control arm (209 mL vs 165 mL). The radiation dose was also significantly higher in the intervention group.
But Tsigkas noted that this did not affect the safety endpoint ― contrast-induced nephropathy ― which was comparable between the two arms.
The intervention was also associated with significantly less procedure time (28 min vs 38 min).
Fewer patients in the combined imaging arm ended up undergoing percutaneous coronary intervention (PCI, 20% vs 29%).
Major adverse cardiovascular events were reduced in the combination arm at both the 5-day follow-up (0% vs 11%) and the 30-day follow-up (5% vs 16%).
Asked how the combination approach may lead to lower event rates, Tsigkas replied that no conclusions about this can be reached until completion of the trial.
But he added: “Taking into consideration the existing outcomes, I believe that the experimental arm, which is a staged approach for these patients, may give the opportunity to the interventional cardiologist to choose more wisely the optimal management. This could be associated with the reduced number of PCI procedures in the experimental arm.”
Tsigkas commented: “We firmly believe that our study will have a noteworthy impact in the management of CABG patients. CCTA could gain more ground as the first diagnostic approach in stable patients with complex CABG surgical procedure, and this approach could be beneficial for patients with unknown anatomy and without a surgical report. A CCTA report could guide interventional cardiologists to perform elective angiography instead of searching grafts.”
The final results will provide guidance toward conducting more focused research in this population, he said, “trying to identify the patients getting more benefit with the combination of CCTA and invasive coronary angiography.”
Tsigkas also pointed out that CCTA in this trial is performed mainly in 64- or 128-slice CT scanners, but newer machines (CT 512-slice scanners) “could increase the diagnostic accuracy, could decrease dramatically the radiation dose, the examination time, and improve the convenience of patients undergoing CCTA.”
Commenting on the study for theheart.org | Medscape Cardiology, Petr Widimsky, MD, University Hospital Kralovske Vinohrady, Prague, Czech Republic, said he did not think the study design was optimal.
“With two angiographies in all patients vs one angiography, they could not expect better outcomes. But better outcomes could be expected if CCTA will remove the need for invasive angiography in those 80% of patients who did not finally undergo PCI,” he stated.
Widimsky suggested that a different design may be one in which the experimental group receives only CCTA as a single, noninvasive, planned procedure, with invasive coronary angiography undertaken only for a selected subgroup of patients in whom combination of clinical presentation and CCTA does not provide a clear decision about a PCI indication.
“With such study design, there would be greater chance to obtain a positive result for the experimental arm,” he said.
Tsigkas responded: “Unfortunately, at the present time, CCTA is not as reliable as invasive coronary artery for native disease assessment; thus, we could not restrict the protocol to CCTA alone.”
He added that a previous nonrandomized study supports the idea of the current combination approach being tested here in terms of contrast and radiation dose, adding that “although patients undergo two rather than one angiography, the invasive one at least lasts significantly less time.”
Tsigkas has disclosed no relevant financial relationships.
Congress of the European Association of Percutaneous Coronary Interventions (EuroPCR) 2022: Presented May 17, 2022.
For more news, follow Medscape on Facebook, Twitter, Instagram, and YouTube.
Source: Read Full Article