The available vaccines against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) are quite effective in preventing Coronavirus disease (COVID-19). However, the SARS-CoV-2 Delta variant is of significant concern because it is highly contagious and can infect vaccinated individuals.
A new study published on the preprint server bioRxiv* explores the mechanism of the Delta variant's high infectivity and suggests a plausible pathway by which the Delta variant could escape from vaccine-induced immunity.
.jpg)
COVID-19 vaccines
The spike protein of SARS-CoV-2 binds to the host cell angiotensin-converting enzyme 2 (ACE2) receptor via the receptor-binding domain (RBD) and is essential for infection. It is used for the development of COVID-19 vaccines. Upon vaccination, neutralizing antibodies against different parts of the spike protein are formed and those directed to RBD block the interaction between RBD and ACE2, thus providing immunity against SARS-CoV-2.
SARS-CoV-2 Delta variant
The Delta variant has several mutations in the spike protein, particularly the RBD and the N-terminal domain (NTD). Mutations in the RBD alone do not make it highly infectious, but it may be due to mutations in NTD. In fact, certain antibodies against NTD can enhance the infectivity of the virus by inducing the open form of the RBD. These are termed enhancing antibodies. Therefore, both neutralizing and enhancing antibodies should be studied to understand the pathogenicity of the SARS-CoV-2 variants.
Why is the Delta variant more infectious?
The researchers from Osaka University obtained anti-spike monoclonal antibodies from COVID-19 patients and analyzed their binding to the Delta spike protein and compared it with wild-type (original virus) spike protein. The anti-spike antibodies were either anti-RBD or anti-NTD; neutralizing or enhancing antibodies; and some anti-NTD antibodies were not well characterized as either neutralizing or enhancing antibodies.
The anti-RBD antibodies bound to Delta spike at levels comparable to wild-type spike. However, anti-NTD neutralizing antibodies could not recognize Delta spike but anti-NTD enhancing antibodies bound to Delta spike at levels comparable to wild-type spike. The anti-NTD antibodies that were not well characterized showed reduced binding or strong binding to the Delta spike.
The researchers also performed in vitro experiments to test the infectivity of the pseudovirus. They used a pseudovirus with Delta spike protein or wild-type spike protein and infected HEK293T cells transfected with ACE2 for virus binding.
The Delta variant escaped from anti-NTD neutralizing antibodies and maintained functional enhancing antibody epitopes suggesting that the Delta variant may maintain infectivity in the presence of anti-RBD neutralizing antibodies because of enhancing antibodies.
Thus, the Delta variant is more infectious, possibly due to mutations in the NTD increasing its antigenicity.
How does the Delta variant escape neutralization by antibodies?
The researchers took sera from healthy individuals vaccinated with the Pfizer-BioNTech BNT162b2 mRNA vaccine. They analyzed the neutralizing activity of these sera against the Delta pseudovirus and compared it with wild-type pseudovirus. In addition to this, they also performed these experiments on pseudovirus containing recombinant spike proteins with different combinations of mutant or wild-type NTD and RBD.
At a high concentration, the immune sera blocked Delta pseudovirus infection but as concentrations were lowered, this blocking decreased significantly compared to wild-type pseudovirus. The neutralizing activity of the immune sera against Delta spike recombinant pseudovirus decreased slightly compared to that of wild-type spike recombinant pseudovirus. It decreased further when wild-type NTD was substituted with the Delta NTD. It was reduced when wild-type RBD was replaced by Delta RBD. It further decreased against Delta NTD.
Taken together, these results suggest that both NTD and RBD mutations in the Delta spike offer resistance against the immune sera.
How do mutations help the Delta variant escape from anti-NTD neutralizing antibodies?
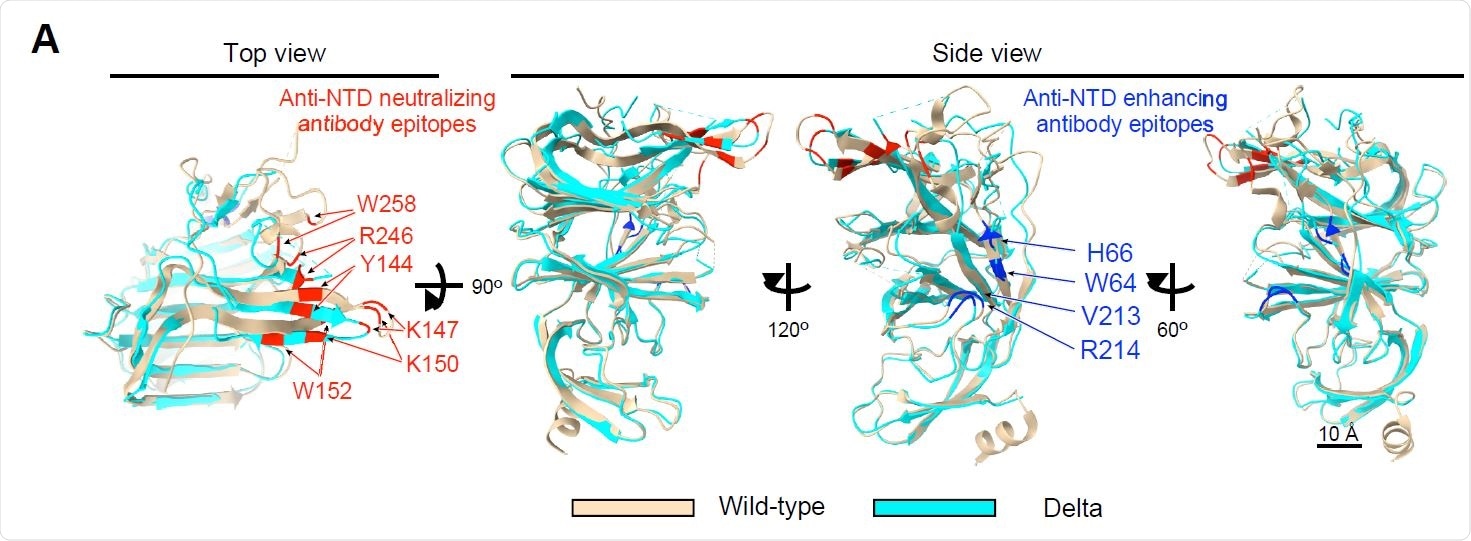
This question was addressed by performing structural analysis of the spike protein by using cryo-EM and assessing the NTD structure.
The data suggested that the structure of the Delta spike protein anti-NTD neutralizing antibody epitope changed dramatically from the wild-type. This structural change caused a complete loss of reactivity of anti-NTD neutralizing antibodies against the Delta spike.
Is it possible that future mutations will make the Delta variant fully resistant?
Additional mutations in the RBD of the Delta variants may make it fully resistant to the immune sera of vaccinated individuals. The researchers obtained data from the GISAID database – complete genomic data of all variants of SARS-CoV-2. They analyzed the additive effects of mutations acquired by the Delta variant. Furthermore, they tested Delta spike protein with additional mutations with monoclonal antibodies, immune sera from vaccinated individuals and the pseudovirus experiments.
Multiple mutations in the Delta variant anti-RBD neutralizing antibody epitopes have already emerged. Mutations in the NTD of the Delta spike made the virus more susceptible to enhancing antibodies and reduced the neutralizing effect of anti-RBD neutralizing antibodies. Thus, the Delta variant is likely to acquire further mutations with increased infectivity and resistance.
Do we need a different vaccine against the Delta variant?
The researchers immunized mice with wild-type (currently available vaccines) or Delta spike protein. While all mice produced antibodies against spike protein, only sera from the Delta-spike immunized mice neutralized the Delta variant with additional mutations without enhancing infectivity.
Therefore, vaccines containing the Delta spike might be required to control the future Delta variants.
*Important notice
bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Liu Y, Arase N, Kishikawa J, et al. The SARS-CoV-2 Delta variant is poised to acquire complete resistance to wild-type spike vaccines. bioRxiv. January 2021:2021.08.22.457114. doi:10.1101/2021.08.22.457114, https://www.biorxiv.org/content/10.1101/2021.08.22.457114v1
Posted in: Medical Research News | Disease/Infection News
Tags: ACE2, Angiotensin, Angiotensin-Converting Enzyme 2, Antibodies, Antibody, Cell, Coronavirus, Coronavirus Disease COVID-19, Enzyme, Genomic, immunity, in vitro, Protein, Pseudovirus, Receptor, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Spike Protein, Syndrome, Vaccine, Virus
Written by
Dr. Shital Sarah Ahaley
Dr. Shital Sarah Ahaley is a freelance medical writer. She completed her Bachelor's and Master's degree in Microbiology at the University of Pune. She then completed her Ph.D. at the Indian Institute of Science, Bengaluru, where she studied the mechanisms of myofibrillogenesis and human myopathies using Drosophila mutants. After her Ph.D., she worked at the Indian Institute of Science, Education, and Research, Pune as a post-doctoral fellow and then continued as a DBT-Wellcome Early Career Fellow.
Source: Read Full Article
