Although there has been significant progress in the treatment of rare forms of blood cancer in recent years and new drugs have been approved in Germany, the prognosis for many affected individuals remains unfavorable. Research teams at Leipzig University’s Faculty of Medicine are working on several preclinical and translational projects to gain a better understanding of these diseases. The researchers are investigating how bone marrow cancer develops. In addition, they have found a new molecular functional mechanism and have shown that patients with even low amounts of leukemia cells have a high risk of relapse.
Why do up to 80% of patients with bone marrow cancer (multiple myeloma) develop bone damage (osteolysis) in some regions of the body while others are spared this damage? This is a question that has not yet been sufficiently investigated. On a research stay in Buffalo, New York, the senior physician PD Dr. Maximilian Merz from Leipzig was able to show that the malignant plasma cells that trigger bone damage differ significantly from the rest of the cells in the body. Using computed tomography-guided punctures, myeloma cells were selectively harvested from osteolyses and studied through single-cell sequencing and other technologies. The samples obtained were then compared with malignant plasma cells from the iliac crest. Bone marrow puncture is usually performed here in routine diagnostics in order to further investigate the malignant cells. Dr. Merz and his team were able to demonstrate that plasma cells from osteolyses elicit genes that, among other things, stimulate bone-degrading osteoclasts and induce new vessel formation. “Our findings underscore the fact that myeloma can have many faces and that several different clones can occur simultaneously in multiple locations in patients. This will have diagnostic, prognostic and therapeutic consequences in the future,” said Dr. Merz summarizing the findings.
New functional mechanism in leukemia of T- lymphocytes investigated
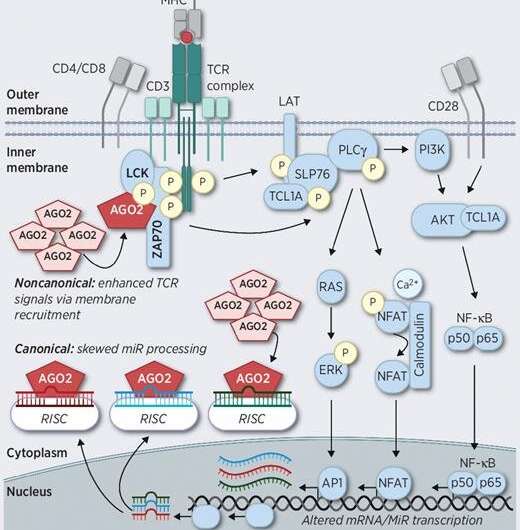
The research group led by PD Dr. Marco Herling discovered a new, molecular functional mechanism of a rare and to date little researched form of blood cancer of the T-lymphocytes. This disease rarely responds to the usual blood cancer therapies and has a poor prognosis with an average patient survival rate of about two years. In their research, Herling’s team found that the molecule AGO2 plays a crucial role in this rare form of blood cancer. AGO2 was previously thought to be a key cancer-initiating molecule that was significantly involved in the fine regulation of normal and tumor gene expression.
“In our research, we were able to decipher a new, unconventional functional mechanism of AGO2 in the leukemia cells,” Dr. Herling said and then added, “AGO2 interacts directly with essential proteins of signal transduction from a very central growth factor of the T-cell, the T-cell antigen receptor. The presence of AGO2 augments the response to incoming cell signals.” This previously unknown molecular interaction was validated using various methods of protein analysis and its high molecular structure was determined. This represents a new medical approach to therapeutic interventions.
Patients with even very small amounts of leukemia cells have a high risk of relapse
For patients with acute myeloid leukemia, bone marrow transplantation is an effective treatment option in certain situations. It is therefore important that physicians identify patients who have a high risk of relapse after transplantation as early as possible during the treatment process. With this knowledge, they can then adjust the treatment options at an early stage.
Source: Read Full Article
