Continued treatment for patients with cancer near end-of-life delays conversations about goals of care and hospice enrollment, escalates costs, and may adversely affect the quality of care patients receive. Accordingly, over the last decade, major professional societies have recommended that clinicians decrease the use of systemic anti-cancer therapies at the end-of-life stage.
In a study published today in JAMA Oncology, researchers at Yale Cancer Center in collaboration with researchers from Flatiron Health, Inc., revealed that despite these recommendations, aggressive cancer care at the end-of-life persists and there has been a substantial transition from the use of chemotherapy to immunotherapy.
“Over the last decade, the landscape of systemic anti-cancer therapy has changed dramatically following the approvals of multiple new targeted therapies,” said Kerin Adelson, MD, Associate Professor of Medicine (Medical Oncology), Chief Quality Officer and Deputy Chief Medical Officer for Smilow Cancer Hospital, and senior author on the study.
“The quality measure that was developed ten years ago by professional oncology organizations, focuses on reducing end-of-life chemotherapy with the goal of providing patients with earlier palliative care. It is unclear whether this has benefited the end-of-life care patients receive.”
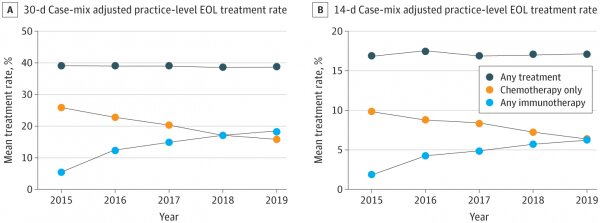
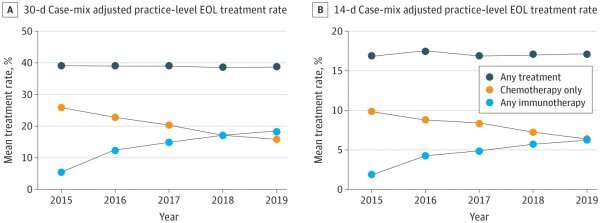
To learn more, the researchers used the nationwide Flatiron Health electronic health record (EHR)-derived database to evaluate adult patients with cancer who received treatment and died within four years of diagnosis. Over the study period, rates of treatment within 30 days of death among all cancer types combined did not change (39% in 2015 and 2019) with similar trends seen for treatment within 14 days of death (17% in 2015 and 2019).
However, the type of systemic therapy received did vary; there were overall decreases in the use of chemotherapy (26% in 2015 and 16% in 2019) and increases in the use of immunotherapy (5% in 2015 and 18% in 2019). These changes were most noticeable in advanced non-small cell lung cancer and urothelial cancers where increases in treatment at end-of-life were driven by increased checkpoint inhibitor use.
Source: Read Full Article