A USC-led team of scientists has found indications that a special blood test called a liquid biopsy could determine whether a patient has breast cancer at its early stage and if that cancer is unlikely to return.
These high-definition comprehensive liquid biopsies are conducted using a standard blood draw from the arm of a patient in a doctor’s office. Once in the laboratory, the sample is examined for signs of cancer.
The study demonstrating the liquid biopsy results for early breast cancer detection was published on Sept. 27 in Nature’s npj Breast Cancer journal. The work was a collaboration between USC, Billings Clinic, Duke University, Epic Sciences and USC Norris Comprehensive Cancer Center. The results raise hopes that one day doctors could detect breast cancer in patients with a simple blood draw.
The researchers at the USC Michelson Convergent Science Institute in Cancer (CSI-Cancer) are cautiously optimistic about their findings. They are eager to test and see whether the results will be proven in larger clinical trials to demonstrate the benefit of the method for patients everywhere.
“It’s an amazing opportunity to change how early breast cancer detection is being done with a simple blood draw, but it’s only a research outcome at this point and we still need to demonstrate clinical benefit,” said Peter Kuhn, a USC cancer physicist who directs CSI-Cancer.
Breast cancer is the most prevalent form of cancer in the world, affecting 1 in 8 women over their lifetime.
Since 1976 when the American Cancer Society endorsed the technique, mammography X-ray, along with a tissue biopsy, has become the standard way for doctors to check patients for breast cancer.
But mammography is not 100% accurate and its detection can be impeded by healthy dense tissue. Mammography’s sensitivity to breast cancer is around 87%, according to the Breast Cancer Surveillance Consortium. And for some women, mammograms are not accessible, especially those living in poor isolated communities that have no clinics or hospitals. Others simply do not get a regular mammogram.
But a tissue biopsy also is not a fool-proof method. Although it can reveal information about the tumor, it has limitations. Doctors can sample only a small area and may fail to capture the full extent of the tumor. A tissue biopsy is also invasive and painful.
Combined, the drawbacks for diagnosis with mammograms and tissue biopsies mean some patients are not diagnosed until the cancer has grown and spread. New methodologies such as CSI-Cancer’s liquid biopsy can bring a complementary toolset into clinical practice.
For the study, Kuhn and his team worked with 100 breast cancer patients—some early and late stage—and 40 patients without breast cancer from April 2013 through January 2017. The work was conducted at clinical sites including at the Norris Comprehensive Cancer Center at Keck Medicine of USC, the Billings Clinic in Montana, Duke University Cancer Institute in Durham, North Carolina and the City of Hope Comprehensive Cancer Center in Duarte, Calif.
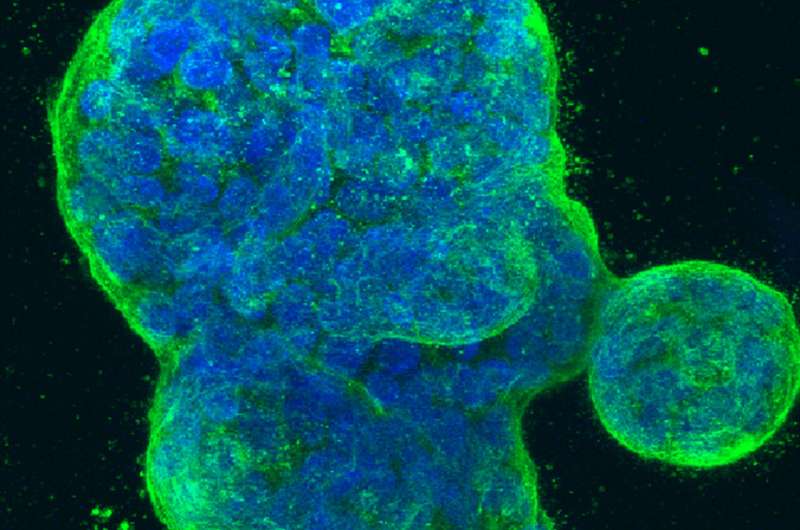
The team tested a theory that the high-definition liquid biopsy could detect multiple cancer biomarkers, including the so-called “oncosomes”—nano-sized, membraned cargo carriers that enrich the body’s environment for cancer growth. These oncosomes are secreted by cancer cells as the group has shown previously.
“The news here is that we found the vast majority of early-stage breast cancer patients have these oncosomes at very robust levels,” said Kuhn, a Dean’s Professor at USC Dornsife College of Letters, Arts and Sciences and cancer physicist. “They’re about 5-10 microns in diameter. About the size of a cell. We first identified these large vesicles in prostate cancer about a year-and-a-half ago and showed that they are related to the cancer. They are hiding in plain sight.”
If further studies produce similar results, this could mean that the next generation high-definition liquid biopsy may become a diagnostic tool for early breast cancer detection and other cancers, he said. The test also could inform patients who have been treated for cancer that they will most likely remain cancer-free.
Source: Read Full Article
