Researchers and clinicians from the School of Biomedical Engineering & Imaging Sciences have for the first time conducted a shape analysis of the fetal aorta to detect a congenital heart defect before birth. Their research was published in Journal of Cardiovascular Translational Research.
Coarctation of the aorta (narrowing of the main body artery) is one of the most challenging conditions to diagnose before birth.
Before birth the arterial duct (a connection between pulmonary artery—blood vessels that carry oxygen-poor blood from the right side of your heart to your lungs—and aorta) is open, directing blood away from the lungs in fetal life. This connection usually closes soon after birth. Then, if the aorta is too narrow (coarctation), it prevents oxygen- rich blood passing through from the heart to the rest of the baby’s body which requires surgery.
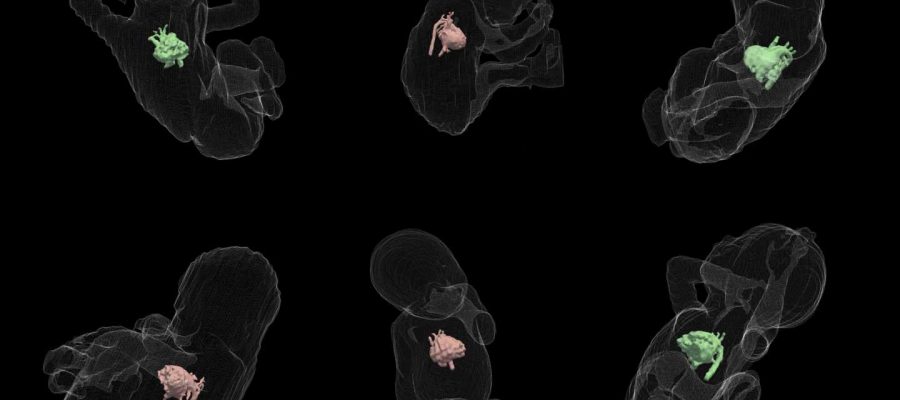
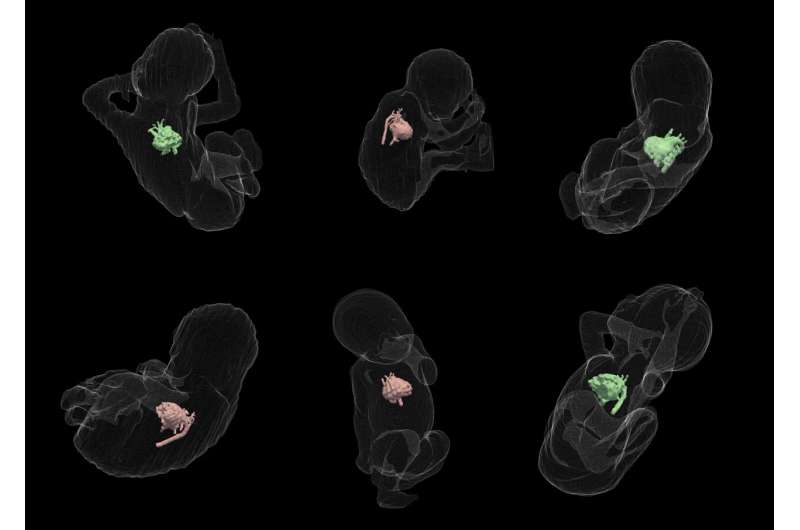
If undiagnosed or misdiagnosed before birth, the baby may have serious problems and may need surgery or other procedures soon after birth. Currently, coarctation of the aorta is diagnosed before birth by echocardiogram (ultrasound pictures of the heart). Fetal cardiac magnetic resonance imaging (MRI) has been shown to help in the diagnosis of coarctation of the aorta in previous work by the team. But this diagnostic information is limited as current techniques only use 2D metrics meaning there is not a full understanding of the complex 3D anatomy.
Lead researchers, Ph.D. students Uxio Hermida and Milou van Poppel, said this new research reveals the detailed 3D anatomy of the fetal aorta that leads to coarctation. This shape analysis is focused on diagnosis but it could also be used to study how the shape changes during the pregnancy. By applying this new method, the researchers hope to improve accurate diagnosis and also reduce false positive diagnoses.
“After the babies are born, the problem is that the arterial duct closes, so the anatomy is different. The arch shape before birth is known to be an important factor to diagnose the condition. However, currently, mostly 2D information is used by clinicians and there is not a deep understanding of the 3D shape changes while babies are in the womb. With our analysis we help clinicians visualize for instance what visual characteristics a false positive case has that is different from a true positive or a negative, which might not be obvious from 2D images,” write Hermida and van Poppel.
False positives account for up to 80 percent of cases in some centers worldwide: with the new shape analysis tools, clinicians could accurately classify with a single risk score which case is more likely to be coarctation or which is more likely to be a false positive while also having a 3D visualization of the aorta.
The researchers say by having this kind of analysis clinicians can now ask questions that were not possible before by using computer simulations to get more insights into why some shapes associated with the condition and others not.
“This important research looks at the underlying signals hidden in the 3D shape of the body artery using prenatal MRI scans, revealing distinct patterns that aren’t immediately obvious to the naked eye. In the future we hope that these shape signals can be combined with other types of antenatal imaging to more accurately predict the condition, so that affected newborn babies have immediate access to the treatment they need,” says Dr. David Lloyd, Consultant in Pediatric and Fetal Cardiology, Evelina London Children’s Hospital and Senior Lecturer in Child Health, School of Biomedical Engineering & Imaging Sciences
More information:
Uxio Hermida et al, Learning the Hidden Signature of Fetal Arch Anatomy: a Three-Dimensional Shape Analysis in Suspected Coarctation of the Aorta, Journal of Cardiovascular Translational Research (2022). DOI: 10.1007/s12265-022-10335-9
Journal information:
Journal of Cardiovascular Translational Research
Source: Read Full Article