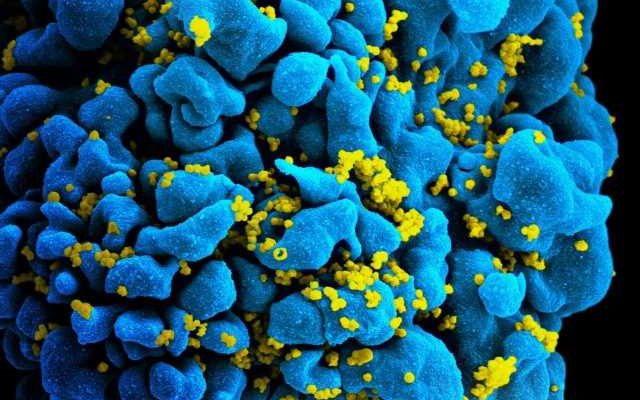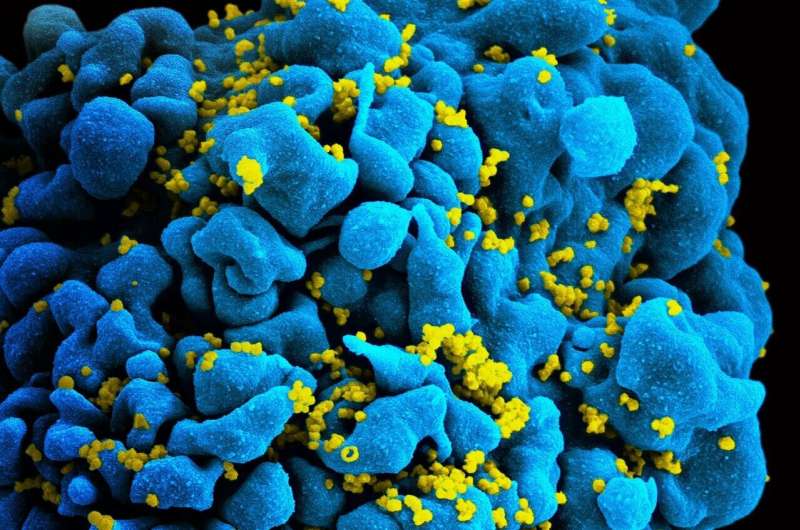
New research from Boston Medical Center found that providing pragmatic support, specifically rapid access to antiretroviral therapy, pharmacotherapy for opioid use disorder, and strengths-based case management, improved treatment outcomes for people with HIV who inject drugs in St. Petersburg, Russia.
Published in The Lancet HIV, researchers from the Linking Infectious and Narcology Care—Part II (LINC-II) trial highlight that the odds of achieving viral load suppression at 12 months are three times higher for participants randomized to the intervention group.
Russia continues to have the largest HIV epidemic in Europe, with the total number of people with HIV exceeding 1.4 million and over 71,000 new infections in 2021. Among the newly diagnosed Russian people with HIV in 2021, 28% reported past injection drug use. Strengthening the HIV response in Russia requires engaging people who inject drugs in treatment. Antiretroviral therapy coverage in Russia is low for people with HIV who inject drugs, and HIV and addiction treatment in Russia are not well integrated.
While the study’s focus was on people with HIV who inject drugs in St. Petersburg, Russia, the implications of early ART initiation extend far beyond national borders.
“We hope to improve the treatment for people with HIV who inject drugs by addressing barriers for accessing both HIV and addiction care, a challenge both in Russia and other countries with this population,” said senior author Jeffrey Samet, MD, MA, MPH, a primary care physician at Boston Medical Center and John Noble, M.D. Professor in General Internal Medicine at Boston University Chobanian & Avedisian School of Medicine. “Scaling up the LINC-II model is one strategy to advance the UNAIDS goal of ending the HIV epidemic.”
These findings support the usefulness of expanding the LINC-II approach in Russia, given both the positive outcomes of the findings and the high receptivity by participants to elements of the intervention.
Researchers believe that although significant improvements were achieved with the intervention, the results do highlight the great challenge of effectively treating people with HIV who inject drugs.
More information:
Jeffrey H Samet et al, Rapid access to antiretroviral therapy, receipt of naltrexone, and strengths-based case management versus standard of care for HIV viral load suppression in people with HIV who inject drugs in Russia (LINC-II): an open-label, randomised controlled trial, The Lancet HIV (2023). DOI: 10.1016/S2352-3018(23)00143-1
Journal information:
The Lancet HIV
Source: Read Full Article