Health departments are predicting another COVID surge related, in part, to more easily transmitted new variants and waning immunity.
Given COVID cases are rising and likely underestimated, Chief Medical Officer Paul Kelly has strongly suggested people wear masks in indoor spaces.
So it’s important to get across how effective they are and which type to choose. Is it worth dusting off last year’s cloth masks, using a surgical mask, or going out to buy some N95 respirators to wear over the coming weeks?
COVID spread and the effects of winter
The SARS-CoV-2 virus (which causes COVID) spreads mainly through breathing in contaminated droplets or aerosols (tiny particles that are left when fine droplets dry out) released into the air when an infectious person breathes, talks, laughs, shouts, coughs or sneezes. This can happen even when they don’t have any symptoms.
Larger droplets fall to the ground quickly, so distancing yourself from others gives you some protection. Aerosols, though, can hang in the air for hours and travel all around a room.
So you can be infected by aerosols indoors even at a distance from an infectious person or after they have left the room.
COVID case numbers tend to increase during winter. This may be because:
- the virus remains viable (able to cause an infection) for longer in cool and less humid conditions
- we tend to remain indoors when it’s cold, and sharing indoor spaces with others increases the risk of contracting COVID.
Which indoor spaces are the most risky?
The most risky indoor settings are:
- places where people are talking loudly, laughing, singing or shouting, because more droplets and aerosols are released
- rooms where ventilation is poor, as the contaminated particles are not being quickly removed
- spaces that are crowded or where you are exposed for a longer period, as the risk goes up with extended contact.
In other words, spending two minutes in a small shop with an open door and one other person present is less risky than sitting in a crowded indoor bar for hours where everyone is talking loudly to be heard over the background noise.
What can I do?
Wearing a mask or respirator can protect you and others in the community from COVID infection. Some people are at greater risk of severe illness due to old age or poorly functioning immune systems.
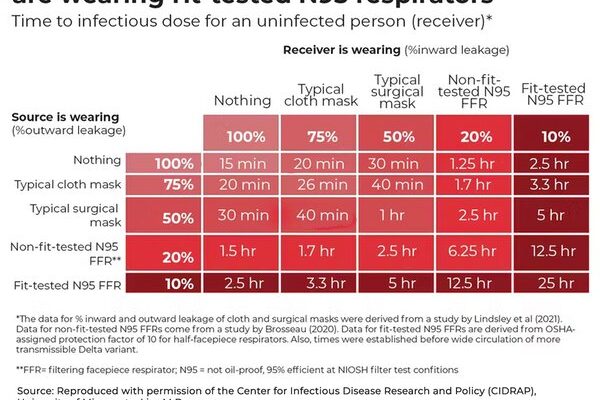
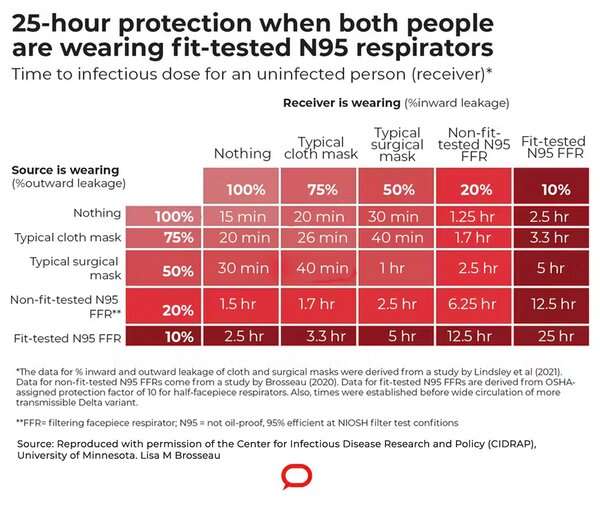
As the table above shows, when both the infected and uninfected person wear a mask or respirator, the protection is greater than if just one of them wears one.
https://youtube.com/watch?v=eAdanPfQdCA%3Fcolor%3Dwhite
What is the difference between a mask and respirator?
Respirators are specifically designed to a standard that prevents 95% of particles from getting through them. So they drastically reduce airborne spread.
Surgical masks are designed primarily to prevent spread of large droplets, so they can stop an infected person spreading disease. This is called source control.
Cloth and surgical masks filter out viral particles by having multiple layers. Respirators (N95s, also called P2s) are more effective at filtering very small particles, because not only do they have multiple fibers, but are made of a type of plastic mesh with a charge that attracts and traps viruses and other particles.
Unlike masks, respirators are also designed to have a tight fit to the face so air enters the lungs only after passing through the respirator. Cloth or surgical masks allow some air entry around the edges because they are not so tightly fitted.
How well do masks and respirators work?
To assess COVID risk and masks, we have to rely on studies in which we are unable to control exactly what people’s exposure to the virus is. This is because we can’t deliberately put people in risky settings. But that means the results are less clear-cut than if we could control the duration and concentration of disease around each subject.
One meta-analysis (pooled results from multiple studies) of the performance of surgical masks versus respirators in healthcare workers found respirators tended to provide better protection than surgical masks, but the difference was not statistically significant. However, staff were more likely to wear respirators when they were working in high-risk areas with greater exposure to COVID, so the results were biased against respirators.
A recent community study compared the effectiveness of masks or respirators with no masks. People who had received a positive COVID PCR result were matched by age, gender and locality, with people who had a negative result. They were surveyed about their mask or respirator use in indoor public settings two weeks before the test.
Those who always wore any type of mask or respirator in indoor public spaces were 56% less likely to test positive than those that never wore one. There was an 83% reduction in the odds of getting a positive test in those who wore a respirator, compared with a 66% reduction in those wearing surgical masks. Those wearing a cloth mask had lower odds of having a positive PCR test result than those wearing no mask, but the difference was not statistically significant.
Those who wore any mask or respirator most of the time had better outcomes than those who wore them some of the time or not at all.
OK, so you’re reaching for a respirator. But which one?
If you are using an N95/P2 respirator, find a brand that fits snugly to your face. Try a few to find one that is most comfortable for you. Note they are not designed for children. And they don’t work well for people with beards, as the hair affects the seal.
Once worn, the respirator is considered contaminated so sanitize your hands before and after handling it, and store it in a paper bag between uses so it can dry out. Don’t reuse the device if it gets dirty, if the straps break or become loose, or if the strip over the nose breaks.
Source: Read Full Article