Californians, starting next year, will be able to access HIV prevention medications without a prescription.
Gov. Gavin Newsom signed a bill into law on Monday, making California the first state in the country to allow post-exposure and pre-exposure prophylaxis to be sold over the counter.
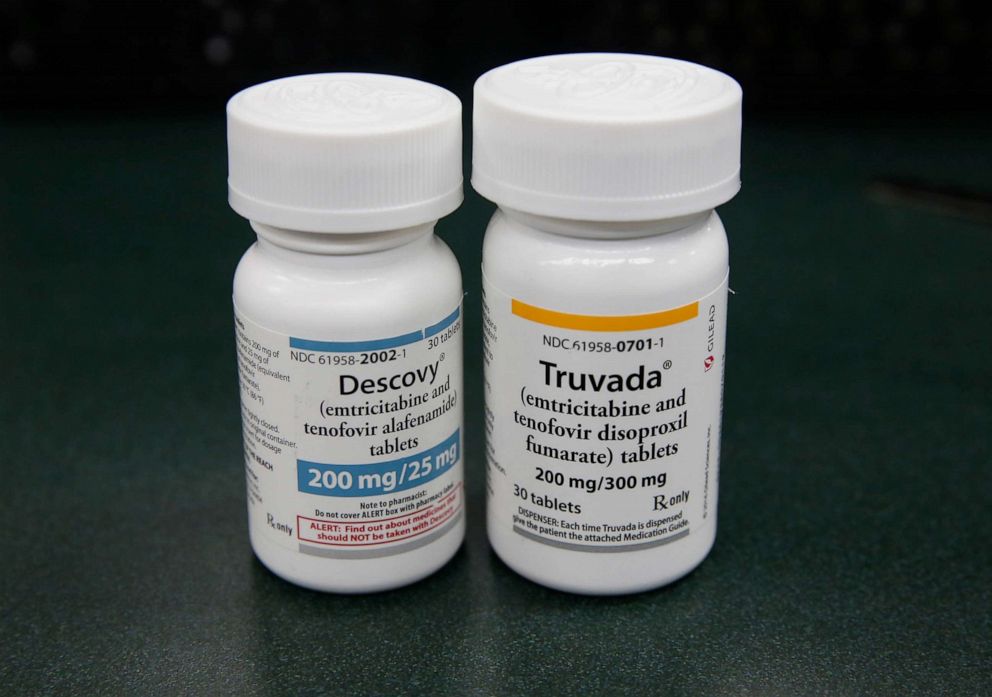
Pre-exposure prophylaxis, known as PrEP, is a once-daily pill that prevents an HIV infection before it occurs. Post-exposure prophylaxis, or PEP, is taken after possible exposure to HIV to avoid contracting the disease. Because PEP is most effective when taken within 72 hours of exposure, requiring a prescription limits access to the time-sensitive medication.
Other barriers to PrEP access include too few doctors prescribing it, PrEP’s high cost and a persistent stigma against people at high risk for HIV, which can make it harder for them to approach providers or discuss with them their sexual health and drug use.
“If we are going to end the epidemic — a goal of the current administration — we need increased access to PrEP,” said Dr. Alysse Wurcel, an infectious disease physician at Tufts Medical Center.
Wurcel said she supported PrEP being available without a prescription and compared the medication to another harm-reduction tool: seat belts.
“When the seat belt first came out, people thought it should not be available, because then people would drive faster and get into more accidents. Could you imagine if someone needed a prescription for a seatbelt?” she asked. “Everyone should have access to harm-reduction tools, whether it be a seat belt, a condom or a pill that prevents HIV.”
A Centers for Disease Control and Prevention analysis last year found that only a small percentage of Americans who could benefit from PrEP are prescribed the medication. Of the people who could potentially benefit from PrEP and don’t have prescriptions, two-thirds are African American or Latino, according to the CDC.
“One of our most powerful tools for HIV prevention remains largely on pharmacy shelves,” Dr. Jonathan Mermin, director of the CDC’s National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, said in a statement at the time of the report.

Two other important tools, according to Wurcel, are sexual health counseling and testing for sexually transmitted infections, both of which should be part of a health care regimen that includes PrEP.
“Sexual health does not stop at access to PrEP. That may be where it starts — where someone feels empowered and takes a pill to protect themselves against HIV — but that should not be where it stops,” Wurcel said.
In 2017, nearly 39,000 people received a new HIV diagnosis, according to the CDC. Of those new diagnoses, men who have sex with men face the highest risk.
In California, pharmacists can already dispense emergency contraception and birth control without a prescription, thanks to laws that went into effect over the last decade.
Source: Read Full Article
