A new discovery from the University of Virginia School of Medicine could let doctors ramp up production of blood-clotting platelets on demand, a timely finding following the Red Cross’ declaration earlier this year of a national blood “crisis.” The group labeled it the worst blood and platelet shortage in more than a decade and said it posed a “concerning risk to patient care.”
In addition to making available more lifesaving platelets for transfusion, UVA’s new discovery could help doctors better treat thrombocytopenia, a potentially dangerous clotting disorder that strikes almost a third of newborns in intensive care. The finding also could benefit patients battling cancer who need cord-blood transplants.
“Because of worsening shortages of donor-derived platelet units, there has been a big push within both public and private sectors for cell culture-based methods of generating platelets,” said Adam N. Goldfarb, MD, the chief of UVA’s Division of Experimental Pathology. “In addition to alleviating platelet shortages, the cell culture approach affords the opportunity for creating ‘designer platelets’—for example, platelets that do not elicit an immune response, which is a major problem in cancer patients.”
Understanding platelet production
The new findings offer important insights into platelet-producing cells called megakaryocytes and how they change between birth and adulthood. In babies, megakaryocytes are much better at proliferating—making more megakaryocytes—than they are at making platelets. It’s like they’re focused on building platelet-production factories. With time, the megakaryocytes begin cranking out platelets in great volume, but this is accompanied by a dramatic slowdown in the production of megakaryocytes. So platelet numbers go up, but the ability to create new “factories” slows to a crawl.
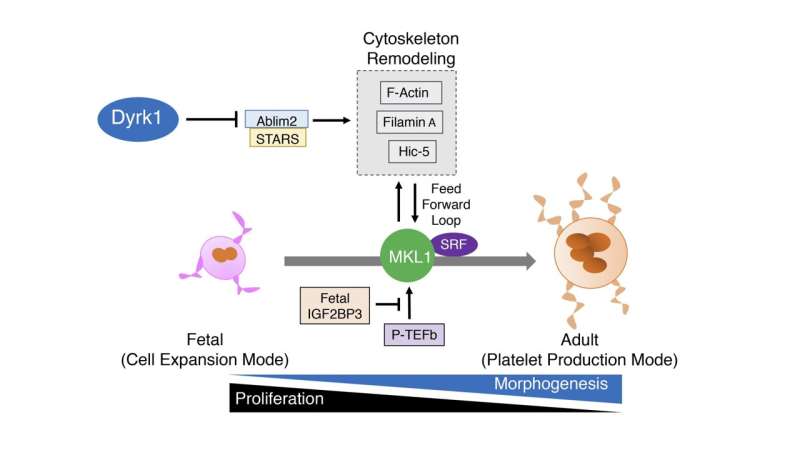
Goldfarb and his team found they could toggle megakaryocytes between their infant and adult modes—between making factories or making platelets—by blocking a particular enzyme, Dyrk1a. Need more factories? No problem. That could relieve a major bottleneck in the production of platelets outside the body for transfusion.
Further, the finding could benefit cancer patients who receive cord-blood transplants by helping overcome platelet problems that slow the immune system’s recovery and raise the risk of dangerous infections. Patients often receive cord-blood transplants when they cannot find a suitable donor for stem-cell transplants. Finding a donor can be especially challenging for people of African, Asian, Hispanic, Middle Eastern, southern European or mixed ethnic backgrounds.
The discovery could also lead to new treatments for thrombocytopenia, a condition in which the body has too few platelets. This can be the result of immune system problems, a bone marrow disorder such as leukemia (blood cancer), some viral infections or the use of certain medications. Thrombocytopenia is a particular problem for premature babies—the more premature the baby is, the more severe the condition tends to be. Many premature babies require platelet transfusions to reduce their risk of uncontrolled bleeding inside the body.
Promisingly, there are already drugs to inhibit Dyrk1a—that could flip the biological switch in megakaryocytes. These drugs are being evaluated to battle diseases ranging from Alzheimer’s to diabetes. The availability of the drugs should speed human trials testing the clinical benefits of manipulating megakaryocytes, the researchers say. “Fortunately, these megakaryocytes can be grown in large numbers from umbilical cord blood cells,” said researcher Kamaleldin E. Elagib, MBBS, Ph.D., of UVA’s Department of Pathology.
Goldfarb, the associate director of UVA Health’s Clinical Hematology Laboratory, notes that the new discovery could have far-reaching benefits. “In the short term, we hope to improve the efficiency of donor-independent platelet production to the point where it could be scaled up for routine clinical use. In the long term, we hope to identify new patient treatments that could stimulate rapid platelet recovery,” he said. “Our findings offer a perfect example of how studying infantile versus adult cell development can yield clinical benefits.”
Source: Read Full Article
