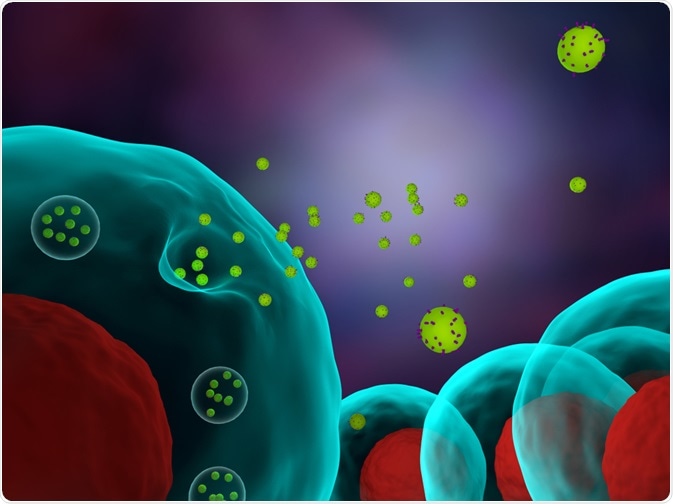
Extracellular vesicles are secreted by many cell types in the body. They exist in various shapes and sizes; for example, exosomes are nanovesicles of size 30–200 nm that are released after fusing with the plasma membrane of intraluminal vesicles.
Other extracellular vesicles include microvesicles that are larger than exosomes and originate from the plasma membrane, rather than the endocytic pathway. In medicine, extracellular vesicles can be used to inform doctors about the pathophysiological state of an individual. This article describes how extracellular vesicles are detected and the development of a robust technique that overcomes previous limitations.
 Meletios Verras | Shutterstock
Meletios Verras | Shutterstock
Detecting extracellular vesicles in urine
Extracellular vesicles are emerging as a diagnostic tool to sample small samples of blood or urine to monitor the state of a disease. Currently, various methods such as ultracentrifugation, precipitation, and density gradient separation are used to enrich extracellular vesicles before characterizing them.
The size and concentration of extracellular vesicles are determined using physical methods, including nanoparticle tracking analysis, and the protein or nucleic acid concentration is determined using conventional methods, such as Western blot and PCR.
The major disadvantage associated with these methods is that they are time-consuming and the screening of a large number of samples is very difficult. One of the challenges to characterize extracellular vesicle is to determine the molecular composition of the vesicles. As there is a lot of cell to cell variability, choosing universal markers can be less efficient. Changes in the composition of extracellular vesicles in the event of tumors, for example, are not very well understood.
Many of the current methods used to characterize extracellular vesicles are limited by the need for a large sample size and/or an enriched sample.
In one study, researchers employed a technique to sensitively detect extracellular vesicles that requires minimal processing of samples. The extracellular vesicles derived from the prostate cancer cell line were first purified by ultracentrifugation. The reconstituted extracellular vesicles had tetraspanins, CD9, and an epithelial cell marker, EpCAM.
Improving the sensitivity of diagnostic methods
The extracellular vesicles were extracted from a cell line of prostate cancer, PC3. One of the important factors is dilution. In biological samples, such as urine the extracellular vesicles may be diluted to a large extent. Extracellular vesicles obtained from plasma or serum of unhealthy samples may also mix with extracellular vesicles from normal tissues. In cases such as this, additional markers for tumor or stress are used to capture the relevant extracellular vesicles.
To achieve high sensitivity of detection, the researchers first analyzed the parameters that were critical to obtain a high signal-to-noise ratio. As the fluorescence detected in a flow cytometer is proportional to the amount of fluorochrome per cell, the maximum signal can be reached if the number of extracellular vesicles is saturated. Thus, to generate an optimal signal, the total number of beads per experiment and the number of extracellular vesicles that contain the epitope need to be established.
The number of extracellular vesicles captured per bead can be calculated by superimposing the extracellular vesicle circle surface on the surface of the bead. Based on this calculation, a 6-micron bead could house 6420 extracellular vesicles.
If a cytometer had 3000–6000 beads, 1.93–3.85×107 extracellular vesicles would saturate the beads. This is in contrast to the 2 to 4 number of antibodies that can bind to T lymphocytes in conditions that are saturating. This allows the fluorescence of beads can be detected even if only half the binding surface is covered by extracellular vesicles.
A robust and reproducible assay
Six-micron sized beads were used for the study and bead aggregates and debris were discarded. A good signal was obtained when extracellular vesicles were incubated with antibody-coated beads for 18 hours. Thus, using antibody-coated magnetic beads, it was possible to detect even the non-abundant proteins with a detection limit that is lower than the Western blot method.
This method can be used to detect extracellular vesicles that express general extracellular markers, such as tetraspanins or specific markers of epithelial cells, such as EpCAM. This method has a greater sensitivity that allows the visualization of markers directly in dilute samples, such as urine.
This method can be a robust and reproducible assay to detect various tumor markers and can be used to determine the presence and progression of the disease without enriching the sample.
Source
Campos-Silva et al. (2019) High sensitivity detection of extracellular vesicles immune-captured from urine by conventional flow cytometry. Scientific Reports volume 9, Article number: 2042 (https://www.nature.com/articles/s41598-019-38516-8)
Further Reading
- All Flow Cytometry Content
- Flow Cytometry Methodology, Uses, and Data Analysis
- Flow Cytometry Techniques used in Medicine and Research
- Flow Cytometry History
- Fluorescence-Activated Cell Sorting
Last Updated: Jul 31, 2019

Written by
Dr. Surat P
Dr. Surat graduated with a Ph.D. in Cell Biology and Mechanobiology from the Tata Institute of Fundamental Research (Mumbai, India) in 2016. Prior to her Ph.D., Surat studied for a Bachelor of Science (B.Sc.) degree in Zoology, during which she was the recipient of anIndian Academy of SciencesSummer Fellowship to study the proteins involved in AIDs. She produces feature articles on a wide range of topics, such as medical ethics, data manipulation, pseudoscience and superstition, education, and human evolution. She is passionate about science communication and writes articles covering all areas of the life sciences.
Source: Read Full Article
