Though survival rates for children diagnosed with cancer are improving, not all children respond to current medical treatments. Cancers in children, adolescents and young adults can be resistant to medical treatments or recur even when initial treatments appear successful.
Findings of a 10-year study led by the Translational Genomics Research Institute (TGen), an affiliate of City of Hope, and in collaboration with the Beat Childhood Cancer Research Consortium, suggest that deeper genomic analysis and therapies that rely on the body’s immune system potentially offer greater patient benefit.
The study, published today in Cancer Research, a journal of the American Association for Cancer Research, used genomic sequencing to analyze 250 solid tumors from among 202 young patients participating in the Beat Childhood Cancer Research Consortium clinical trials at more than 40 U.S. hospitals and universities. Cancer is the nation’s primary disease-related cause of death among children.
The study focused on those children and young adults whose cancers were refractory, meaning resistant to treatment, or relapsed, meaning the cancer returns following a period of initial improvement. Researchers found that refractory or relapsed tumors had a higher number of genetic mutations than tumors at diagnosis. More than two-in-five tumors mutated as a result of chemotherapy.
“Sometimes, despite the best medical care and the significant progress made in recent years in treating cancer, tumors come back,” said Sara Byron, Ph.D., an Associate Professor in TGen’s Integrated Cancer Genomics Division, and one of the study’s lead authors. “Relapses likely occur because the initial treatments fail to eliminate some of the original cancer cells. We need to know why this happens, and identify ways to more effectively treat these tumors.”
Will Hendricks, Ph.D., an Assistant Professor in TGen’s Integrated Cancer Genomics Division, and another of the study’s lead authors, said this study—with its high demand for computer speed and computational power—was only possible because of a multi-institutional effort and the critical support of Dell Technologies.
“This landmark study provides unique insights gleaned from deep genomic analysis of some of the most clinically challenging tumor types in children,” Dr. Hendricks said.
Partnering with Dell Technologies, TGen reduced computational processing time for these tumor analyses down from weeks to hours. This was instrumental in providing timely results for the patients and their oncologists. The power of applying the latest technologies to help decode the complexity of the human genome continues to propel better treatments for patients.
Of the 202 patients whose cancers were sequenced, 20 patients had multiple recurrences of their cancer, allowing their tumor genomes to be sequenced at each recurrence. This helped reveal the evolution of genetic changes in their cancer over time, and in several cases, revealed new targeted therapeutics.
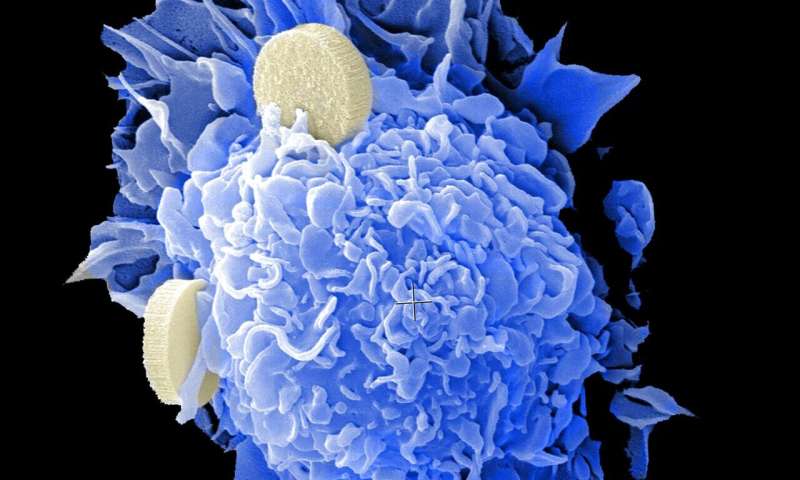
Jeffrey Trent, Ph.D., TGen President and Research Director, and one of the study’s senior authors, noted that many of the children’s cancers displayed various mechanisms of immune evasion and generally showed an absence of infiltration by immune cells, though this finding could potentially open the door to additional research that could identify and develop new therapeutic options.
“Between the potential for targeted therapies, and new ways of leveraging the immune system against cancers, we are encouraged by the potential to use the information found in our study to help these children, giving them and their families answers and hope for the future,” said Dr. Trent, who also directs TGen’s Genetic Basis of Human Disease Division.
The study’s other senior author, Giselle Saulnier Sholler, M.D., agreed, adding that most of the patients in this study had tumors that expressed multiple neoantigens, which are proteins on the surface of tumor cells that can be used as therapeutic targets. More than half of the patients in the study expressed five or more neoantigens.
“This research highlights the importance of genomic sequencing for pediatric cancers at each progression as we gain understanding of how tumors mutate over time and mechanisms of resistance, which may have important clinical implications,” said Dr. Sholler, Director of the Isabella Santos Foundation Solid and Rare Tumor Program at Atrium Health Levine Children’s, where she is a Professor of Pediatric Oncology. Dr. Sholler is chair of the Beat Childhood Cancer Research Consortium.
Javed Khan, M.D., Deputy Branch Chief of the Genetics Branch, and Head of the Oncogenomics Section, at the National Institutes of Health, National Cancer Institute, Center for Cancer Research, noted the complex nature of the study that covered 46 diagnostic types of highly aggressive pediatric cancers, and is a culmination of extensive multi-year collaborations between academia, industry and government.
Source: Read Full Article
