Thrombolytics, intravenous or catheter-directed, can be an effective treatment option for acute pulmonary embolism (PE) but pose a hazard to the many patients who have risk factors for serious bleeding. Thrombectomy catheters of varying designs are available for removing the clots causing PE, but it’s an interventional arena with scant randomized trial data for guidance.
At least one such device performed well enough in an “all-comers” registry study of patients with acute PE to catch the attention of experts at the recent Transcatheter Cardiovascular Therapeutics (TCT) 2022 conference and get them cautiously looking forward to the outcome of a recently launched randomized trial.
Patients with acute PE treated with the FlowTriever mechanical thrombectomy system (Inari Medical) within the prospective FLASH registry showed a 30-day mortality under 1% and rate of treatment-related complications less than 2%. Their 30-day rate of readmission for any cause was 6.2%.
Nearly all the study’s 799 patients were considered intermediate-to-high risk by accepted criteria and a third had absolute or relative contraindications to thrombolytics.
“This is a real-world patient population with elevated markers of risk,” yet mortality was far lower than registry data on conventional acute PE therapy would suggest, said Catalin Toma, MD, University of Pittsburgh Medical Center Heart and Vascular Institute, when presenting the study September 18 at the TCT sessions.
“Most importantly, hemodynamics improved acutely on the table, paralleled by an improvement in vitals and right-ventricular strain,” said Toma, who is also lead author on the data’s same-day publication in EuroIntervention.
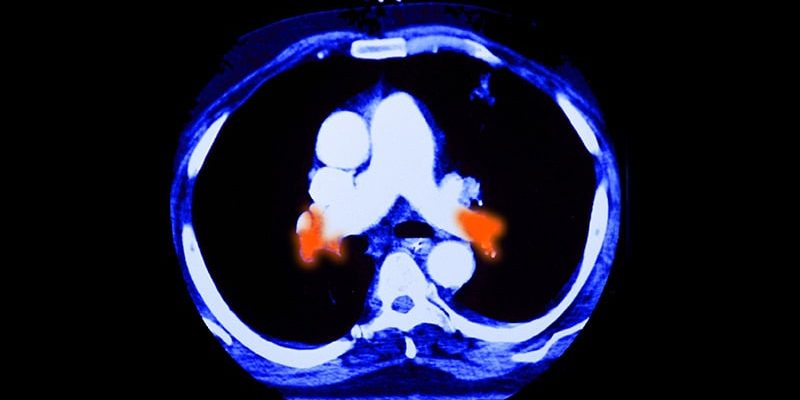
The FlowTriever system, as described in the published report, consists of an aspiration catheter and separate catheter for “mechanical dislodgment and removal” of thrombi without the need for thrombolytics. A proprietary blood return device became available for the system late in the registry accrual.
The system has 510(k) clearance in the United States and the CE mark in Europe for removal of clot from the peripheral vasculature, including in acute PE, according to Inari Medical. But it doesn’t have a randomized-trial track record against pharmacologic or other catheter-based therapies for acute PE.
“It will be interesting to see how this performs against routine clinical care, which in most cases is either thrombolysis or heparin,” Felix Mahfoud, MD, Saarland University Medical Center, Hamburg, Germany, told members of the media at a briefing on FLASH before the formal presentation.
“I think studies are urgently required where these two strategies are compared in a randomized controlled fashion. And then you can look into hard outcomes,” Mahfoud said. “Thirty-day mortality, 7-day mortality, intensive care unit stay — all these are relevant endpoints in these very sick patients.”
The device’s performance in FLASH “is a really important step forward with a different way of approaching the problem, without giving antithrombotic drugs,” said Robert Bonow, MD, Northwestern University, Chicago, Illinois, at the same press conference. But, he agreed, “We really need randomized trials to see where this is headed.”
Systemic thrombolysis, the most common advanced therapy for acute PE beyond conventional anticoagulants, poses a bleeding risk of about 10% or more compared to the 1.4% major bleeding risk observed in FLASH, Toma told theheart.org | Medscape Cardiology.
“That’s exactly why this mechanical thrombectomy presents an advantage.” Also, Toma said, “a third of the patients wouldn’t even have been able to get thrombolysis.”
The overall 30-day rate of major bleeding across more than 400 patients with acute PE in a recent National PERT Consortium multicenter registry study was 13%. Unadjusted rates were 24% in high-risk patients and 9% in intermediate-to-high risk patients. Systemic thrombolysis pushed the risk to 17% and catheter-directed thrombolysis to 19%.
There are at least theoretical risks from using aspiration catheters to remove clot associated with acute PE, Ajay J. Kirtane, MD, SM, Columbia University Irving Medical Center, New York-Presbyterian Hospital, New York City, told theheart.org | Medscape Cardiology.
“With all these devices, because you’re sucking out clot, you’re also sucking blood, so you can have drops in hemoglobin,” Kirtane observed. Even if the aspirated blood is returned to the patient, it’s unknown whether the sheared red cells function properly, he said. “That’s another reason why these randomizations are needed, going forward.”
The registry study followed 799 patients at 50 US sites, 54% of whom were male. About 8% had high-risk massive PE and the remaining 92% at intermediate risk had submassive PE by European Society of Cardiology criteria, states the published report. Deep vein thrombosis was present in 65%.
“A very important aspect of this therapy is that it can provide very quick and rapid improvement in hemodynamics. This was paralleled by an improvement in heart rate — these patients were very tachycardic at baseline,” Toma said at the press conference.
Indeed, as he reported, the treated patients rapidly showed, on average, a 23% drop in mean pulmonary artery pressure and 20% decline in total pulmonary vascular resistance compared to baseline. And the cardiac index rose 19% among those initially with a low index. The changes were all significant at P < .0001.
The study’s primary endpoint of major adverse events (MAE) occurred in 1.8% of patients; it consisted of device-related mortality or major bleeding within 48 hours or device- or procedure-related adverse events. Major bleeding events developed in 1.4%; there were no intracranial bleeds. About 37% of the cohort spent at least one night in the intensive care unit after the acute procedure.
At baseline, Toma reported at the TCT sessions, 15% of patients had normal right ventricular function; the proportion grew to 40% at 48 hours (P < .0001) and to 92.7% “at the latest follow-up.”
The prevalence of severe dyspnea fell from 66.5% at baseline to 15.6% at 48 hours, 6.1% at 30 days, and 2.9% at 6 months (P < .0001 for each improvement step).
The FLASH registry “was designed as a continuation” of the FLARE investigational device exemption study, reported 4 years ago, so as to allow enrolment of “a higher-risk group of real-world PE patients,” Toma said.
FLASH is also a prelude to the recently launched randomized PEERLESS clinical outcomes trial comparing the FlowTriever system to catheter-directed thrombolysis in an estimated 550 patients with acute PE. The trial has a prospective registry component for patients with absolute contraindications to thrombolytics.
Plans for other randomized trials comparing mechanical thrombectomy to conventional anticoagulation therapy for acute PE, Toma said, are “in the works.”
The FLASH registry was funded by Inari Medical. Toma has disclosed serving as a consultant for Medtronic and Philips; disclosures for the other authors are in the report. Mahfoud has disclosed receiving grants or holding research contracts with Medtronic and Recor; and receiving honoraria or consulting fees or serving on a speaker’s bureau for Medtronic, Recor, and Inari Medical. Bonow has disclosed no relevant financial relationships. Kirtane has reported receiving institutional funding from Medtronic, Boston Scientific, Abbott Vascular, Amgen, CSI, Philips, ReCor, Neurotronic, Biotronik, Chiesi, Bolt Medical, Magenta Medical, Canon, SoniVie, Shockwave Medical, and Merck; consulting for IMDS; and receiving travel and meal expenses from Medtronic, Boston Scientific, Abbott Vascular, CSI, Siemens, Philips, ReCor Medical, Chiesi, OpSens, Zoll, and Regeneron.
Transcatheter Cardiovascular Therapeutics 2022. Late-Breaking Clinical Science in Vascular Disease and Hypertension: Session III, in Collaboration with the Journal of the American Medical Association. Presented September 18, 2022.
EuroIntervention. Published online September 18, 2022. Full Text
Follow Steve Stiles on Twitter: @SteveStiles2. For more from theheart.org | Medscape Cardiology, follow us on Twitter and Facebook.
Source: Read Full Article