The coronavirus disease 19 (COVID-19) pandemic, which was caused by the emergence of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has adversely impacted the health of people throughout the world. To date, over 584 million have been infected with SARS-CoV-2, of whom over 6.4 million have died.
The clinical symptoms of COVID-19 can range from cough, fever, and sore throat to mild or severe pneumonia and acute respiratory distress syndrome (ARDS).

Study: Rational development of a combined mRNA vaccine against COVID-19 and influenza. Image Credit: taa22 / Shutterstock.com
Background
The spread of other epidemic respiratory diseases during the cold season increases the risk of co-infections with two or more respiratory pathogens.
One of the most common respiratory pathogens is the influenza virus, which has previously been reported to co-infect with SARS-CoV-2. Both these viruses have similar transmission routes and cause comparable clinical symptoms after infection.
Several recent studies have suggested that influenza infection can facilitate the entry of SARS-CoV-2 inside host cells, subsequently leading to severe pneumonia and lung lesions. Co-infection with influenza and SARS-CoV-2 has also been reported to cause severe weight loss and a higher number of deaths in mammals. Therefore, there is an urgent need to develop a combined vaccine capable of providing protection against both SARS-CoV-2 and influenza.
Recently, messenger ribonucleic acid (mRNA)-based vaccines with a lipid nanoparticle (LNP) delivery system have been used to mitigate the spread of SARS-CoV-2. Several mRNA vaccine candidates against influenza and other respiratory diseases are currently under different developmental stages.
A new npj Vaccines study describes the efficacy of an mRNA vaccine referred to as ARIAV that encodes the hemagglutinin (HA) antigen of influenza A virus (IAV) H1N1. ARIAV was then incorporated into a previous LNP-encapsulated mRNA (mRNA-LNP) vaccine (ARCoV) that encodes the SARS-CoV-2 receptor-binding domain (RBD) to design a combined vaccine formulation referred to as AR-CoV/IAV.
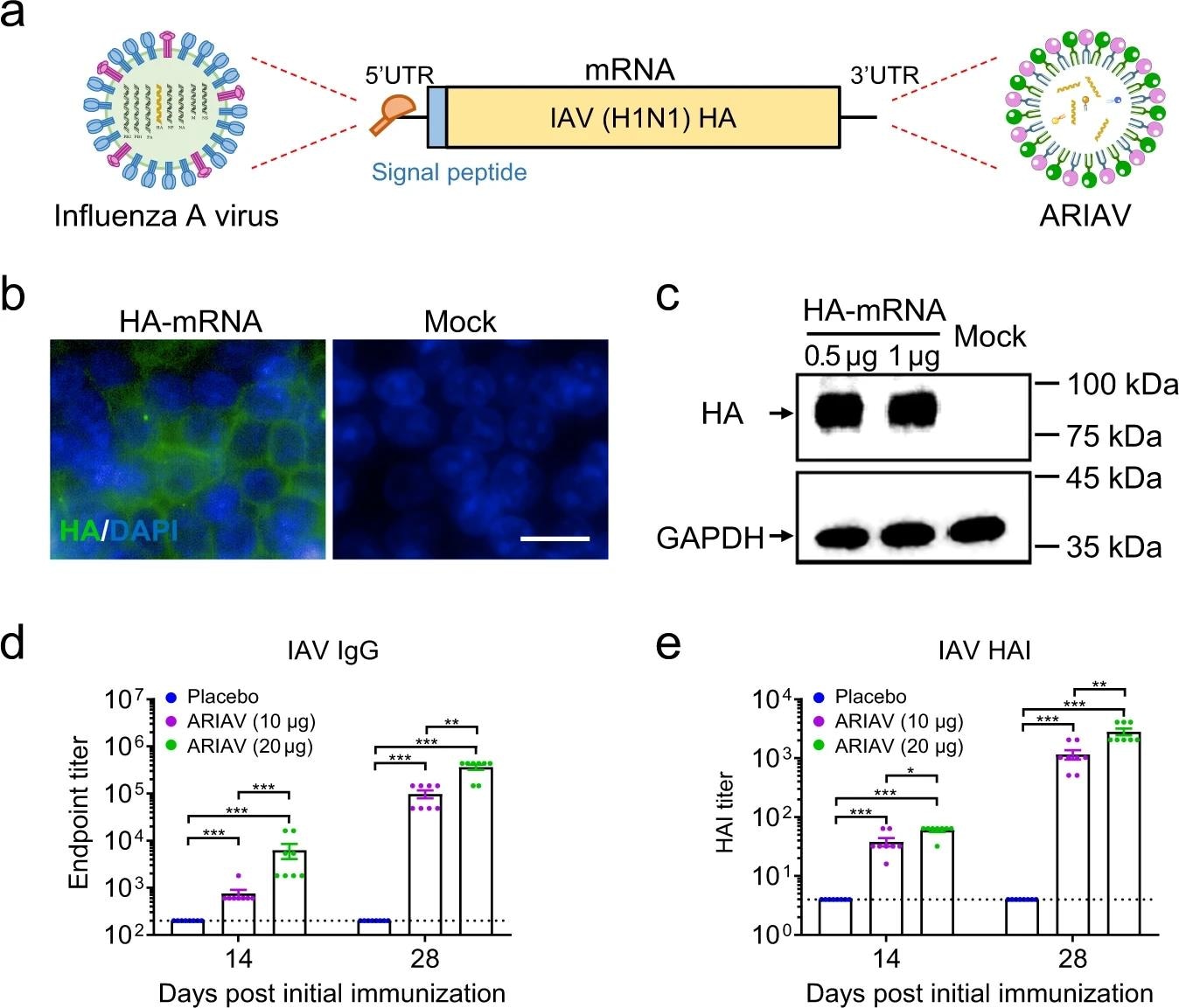 Design and characterization of ARIAV mRNA-LNP encoding HA protein of influenza A (H1N1) virus as a vaccine candidate. a Schematic diagram of ARIAV, encoding the full-length HA protein. b Indirect immunofluorescence assay of HA protein expression in HEK293T cells 48 h post-transfection. Scale bar, 20 μm. c HA expression in HEK293T cells was determined by immunoblotting. d HA-specific IgG antibody titers were determined by ELISA. e Hemagglutination inhibition (HAI) titers were determined 14 and 28 days post-initial immunization. Data are shown as the mean ± SEM (n = 8). Statistical differences were analyzed by using two-tailed unpaired t tests. *P < 0.05,**P < 0.01, ***P < 0.001.
Design and characterization of ARIAV mRNA-LNP encoding HA protein of influenza A (H1N1) virus as a vaccine candidate. a Schematic diagram of ARIAV, encoding the full-length HA protein. b Indirect immunofluorescence assay of HA protein expression in HEK293T cells 48 h post-transfection. Scale bar, 20 μm. c HA expression in HEK293T cells was determined by immunoblotting. d HA-specific IgG antibody titers were determined by ELISA. e Hemagglutination inhibition (HAI) titers were determined 14 and 28 days post-initial immunization. Data are shown as the mean ± SEM (n = 8). Statistical differences were analyzed by using two-tailed unpaired t tests. *P < 0.05,**P < 0.01, ***P < 0.001.
About the study
The study involved the synthesis of mRNA that encoded the full-length HA of IAV and the SARS-CoV-2 RBD, followed by LNP formulation of the mRNA and transfection. Six- to eight-week-old female BALB/c mice were immunized with equal doses of ARIAV, AR-CoV/IAV, or placebo, which was followed by a booster dose 14 days later.
Serum samples were collected from the mice before administration of the vaccines, as well as 14 and 28 days post-administration. Some of the mice were sacrificed post-challenge with either of the viruses or co-infection with both viruses for histopathological analyses and viral detection.
The enzyme-linked immunosorbent assay (ELISA) was used for the detection of SARS-CoV-2- and IAV-specific IgG antibodies. Thereafter, pseudovirus-based neutralization assay, hemagglutination inhibition (HAI) assay, enzyme-linked immunospot (ELISPOT) assay, and multiplex immunofluorescent assay were conducted.
Total RNA was isolated from infected mice and quantified by the quantitative reverse transcription-polymerase chain reaction (qRT-PCR) assay, followed by in situ hybridization assay. Flow cytometry was also carried out, followed by histopathological, cytokine, chemokine, and phylogenetic analyses.
Study findings
ARIAV was found to induce an HA-specific IgG antibody response, as well as an increase HAI titers that continued to rise after booster immunization in a dose-dependent manner. Immunization with two doses of AR-CoV/IAV provided protection against IAV and SARS-CoV-2 infection.
AR-CoV/IAV was observed to activate antigen-specific CD4+ and CD8+ T-cell responses, along with the secretion of several cytokines, including interleukin-2 (IL-2), tumor necrosis factor- α (TNF-α), and interferon γ (IFN-γ).
Histopathological analysis revealed pathological changes in the lung sections following IAV and SARS-CoV-2 infections in the placebo group. However, no pathological changes were observed in AR-CoV/IAV vaccinated mice following infection.
High levels of viral RNA were detected in both IAV- and SARS-CoV-2- infected mice receiving the placebo vaccine post-infection. AR-CoV/IAV immunization reduced the viral RNA load post-infection and conferred protection against IAV and SARS-CoV-2 infection.
Furthermore, AR-CoV/IAV immunization protected infected mice from severe weight loss. This vaccine was also found to protect against infection with the SARS-CoV-2 Alpha and Delta variants. Additionally, AR-CoV/IAV vaccination reduced the levels of proinflammatory cytokines and chemokines, as well as provided protection against IAV and SARS-CoV-2 co-infection.
Conclusions
The current study demonstrated that a combined mRNA vaccine is capable of inducing broad and durable protection against co-infection with SARS-CoV-2 and IAV, as well as against multiple SARS-CoV-2 variants. Further development of universal vaccines is important to control the COVID-19 pandemic, as well as the spread of other respiratory viruses.
- Ye, Q., Wu, M., Zhou, C., et al. (2022). Rational development of a combined mRNA vaccine against COVID-19 and influenza. npj Vaccines 84. doi:10.1038/s41541-022-00478-w.
Posted in: Drug Discovery & Pharmaceuticals | Medical Science News | Medical Research News | Disease/Infection News | Pharmaceutical News
Tags: Acute Respiratory Distress Syndrome, Antibodies, Antibody, Antigen, Assay, CD4, Cell, Chemokine, Chemokines, Cold, Coronavirus, Coronavirus Disease COVID-19, Cough, Cytokine, Cytokines, Cytometry, Efficacy, ELISA, Enzyme, Fever, Flow Cytometry, H1N1, Hybridization, Immunization, Influenza, Interferon, Interleukin, Interleukin-2, Messenger RNA (mRNA), Nanoparticle, Necrosis, Pandemic, Placebo, Pneumonia, Polymerase, Polymerase Chain Reaction, Pseudovirus, Receptor, Respiratory, Ribonucleic Acid, RNA, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Sore Throat, Syndrome, T-Cell, Throat, Transcription, Transfection, Tumor, Tumor Necrosis Factor, Vaccine, Virus, Weight Loss

Written by
Suchandrima Bhowmik
Suchandrima has a Bachelor of Science (B.Sc.) degree in Microbiology and a Master of Science (M.Sc.) degree in Microbiology from the University of Calcutta, India. The study of health and diseases was always very important to her. In addition to Microbiology, she also gained extensive knowledge in Biochemistry, Immunology, Medical Microbiology, Metabolism, and Biotechnology as part of her master's degree.
Source: Read Full Article
