The Texas Heart Institute (THI) has announced that a research team led by Dr. Mehdi Razavi, Director of Electrophysiology Clinical Research & Innovations, has developed a breakthrough new ex vivo benchtop system for evaluating the effects of ablation systems on excised tissues and assessing potential damage to collateral heart tissues. The unique system allows for fast and easy benchtop assessments rather than using costly in vivo tests. Critical findings associated with this innovation are outlined in a study published in the Journal of Cardiovascular Electrophysiology.
The new ablation method evaluated by Dr. Razavi and team is being assessed and used clinically as a promising development to combat the challenge of reducing atrial esophageal fistulas—which are uncommon but often deadly late-stage complications of atrial fibrillation ablation procedures that result from massive thermal injury to the esophagus and surrounding components. Atrial fibrillation (AF) is the most common sustained heart rhythm disorder in clinical cardiology practice worldwide.
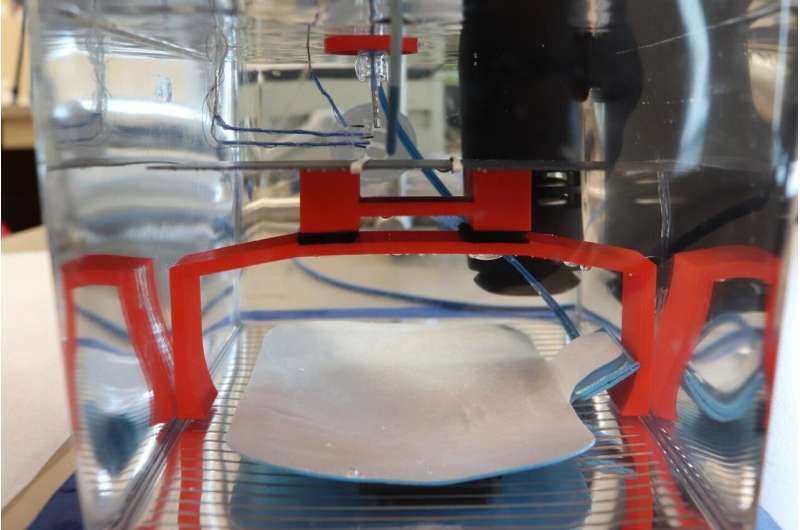
“We created this custom, simple, easy to use fixture to study different ablation settings and the collateral impact of the ablation on the surrounding tissues. It has been useful not only in this particular study, but in many of our other projects as well. It’s quite versatile,” said Mathews John, Dr. Razavi’s Research Engineer III at THI.” Our expertise in ablation and access to an extensive set of ablation equipment enabled us to do these experiments in a way that truly mimics what actually happens in a clinical setting.”
The most critical finding of the study is that High Power Short Duration (HPSD) ablation protocols may be associated with greater epiesophageal thermal deviations relative to endoluminal measurements. The inaccuracy, in turn, raises the threat of downstream clinical consequences. The results of this ex vivo study support the need for esophageal temperature monitoring, particularly during HPSD ablation.
“Electrophysiology doctors have been utilizing this method previously, but no one has really taken a closer look at the full scope of thermodynamics in play during ablation operations,” Dr. Mehdi Razavi noted. He added, “Current technology does not monitor temperature outside of the esophagus during the procedure; it can only monitor temperature changes inside the esophagus itself, which is significant given the fact that major temperature changes occur outside of the organ. To that end, our study sheds light on the problem related to the lack of ability to comprehensively track temperature during these types of procedures and presents an ex vivo method for mitigating this setback.”
The study setup detailed in the manuscript was easily modifiable for collaborations with outside companies to evaluate their new devices in order to help them better gather thermodynamic data and validate potential users of the novel technology.
“Overall, our publication demonstrates very interesting findings from the comparison of two different commonly used ablation methods that have been evaluated using this benchtop system and highlights safety measures that should be considered in a clinical setting. The THI Electrophysiology Clinical Research & Innovations team is excited to use this system for further evaluation and characterization of novel cutting-edge ablation systems,” Dr. Razavi concluded.
Source: Read Full Article
