As dozens of countries blocked the flow of people and goods from Britain to avoid a new and more contagious strain of coronavirus, scientists raced to understand how it emerged and the scope of its threat.
Here are some of the key questions they are asking, and the answers that have emerged so far.
How often do viruses mutate?
All the time, but some viruses do it more than others.
A two-dose vaccine against measles, for example, can last a lifetime, where as the cocktail in flu shots changes every year to keep up with genetic shape-shifting.
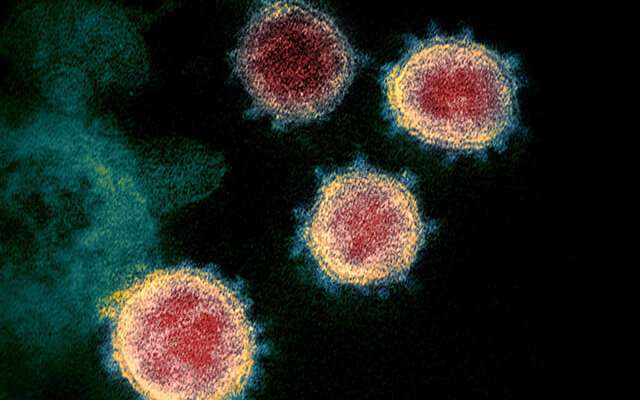
Coronaviruses are somewhere in between, and the one that has ravaged the globe this year, known as SARS-CoV-2, is no exception.
“Viruses constantly change through mutation and the emergence of a new variant is an expected occurence and not in itself a cause for concern,” The European Centre for Disease Prevention and Control (ECDC) said Sunday in an threat assessment report of the new strain.
As for the pathogen that causes COVID-19, “even by March, there were eight major lineages that were all separating,” Susan Hopkins, a senior lecturer in infectious diseases at Imperial College London, told journalists in a Zoom press conference Monday.
The more critical question is where in the virus such mutations occur, and whether they will make it more infectious and/or deadly.
Before the emergence in Britain of this more contagious strain, other genetic variations were mostly benign.
How has the new strain changed?
Whether a variant of SARS-CoV-2 finds a host to infect is significantly determined by the interface between a virus’s so-called spike protein and a specific receptor on the surface of many human cells known as ACE2.
The easier it is for the virus to latch on to a receptor, the more likely it is infection will follow.
The new mutation, known as the 501Y variant, may have changed in ways that enhance its chances of a successful docking.
“There is an really unusual cluster of mutations associated with this variant—22 coding changes across the whole virus genome,” said Wendy Barclay, head of the department of infections disease at Imperial College London and a member of NERVTAG, a group of scientists advising the British government on the threat posed by emerging respiratory diseases.
Mutations observed in the spike protein, she told journalists, “would make it easier for the virus to enter cells, and could biologically explain an increase in transmission.”
Bits of missing genetic code in other regions, compared with the previous generation of SARS-CoV-2 from which 501Y emerged, could also boost its ability to spread, she said.
How much more infectious?
In announcing more stringent lockdown measures over the Christmas holiday, British Prime Minister Boris Johnson said on Saturday the new viral strain “may be up to 70 percent more transmissible than the original version of the disease.”
That assessment was based on preliminary data from sequenced virus genomes gathered from London and parts of southeastern England.
In early November, scientists found the new variant was responsible for just over a quarter of infections in these areas. By the week ending on December 9, it accounted for more than 60 percent of all new cases.
Since Johnson’s shock announcement, which triggered commercial flight bans and border closings, scientists in Britain have crunched even more data.
“We now have high confidence that this variant does have a transmission advantage over other virus variants that are currently in the UK,” said Peter Horby, a professor of emerging infectious diseases at the University of Oxford and chair of NERVTAG.
The latest calculations, he added, suggest 501Y is 50 to 70 percent more infectious.
Another indicator of its ability to spread is the variant’s reproductive number, or “R rate”—the average number of new cases generated by an single infected person.
Anything above 1.0 means that a virus is continuing to find new hosts and is expanding across a community, county or country.
“Even during the (recent) lockdown in England, this virus had an R-number that was about 0.4 larger than non-variant strains,” said Neil Ferguson, director of the MRC Centre for Global Infectious Disease Analysis and a member of NERVTAG.
“The non-variant strains had an R number of about 0.8, but this variant had an R of 1.2 or even higher.”
That could be bad news for efforts to curb the spread of COVID-19, which has already claimed more than 67,000 lives in Britain and 1.7 million worldwide.
“I think it is highly likely to become the dominant strain across the UK given the trends we have seen so far,” Ferguson said.
The World Health Organization (WHO) on Tuesday said that “initial analysis indicates that the variant may spread more readily between people,” but said more research was needed to assess its impact on treatments and vaccines.
Where did the new strain emerge?
Scientists are not sure where the more contagious variant—officially known as SARS-CoV-2 VUI 202012/01—first appeared, but many suspect Britain is ground zero.
The first known case there was sampled on September 20.
“It is very likely that it emerged here, but it is also likely that it is in other countries,” said Hopkins of Imperial College London.
Denmark, The Netherlands, Australia and Italy have all reported cases, she said.
A variant with some of the same genetic deletions has also been identified in South Africa, but is thought to have evolved separately—bolstering the idea that the mutations confer a “transmission advantage”.
It is also possible, scientists say, that 501Y is already more widespread than thought, but has simply not been detected.
The only way to spot a mutated version of SARS-CoV-2 is to sequence the virus’s entire genome, but Denmark and Britain are the only countries in Europe that do so on a routine basis.
“The UK may be victims of their own technical success in highlighting the emergence of the 501Y variant,” said London School of Hygiene & Tropical Medicine Professor Brendan Wren, noting that Britain may be treated “as the lepers of the world.”
Horby and other NERVTAG scientists said Monday they are unlikely to trace the strain back to a “patient zero”, but have an idea of how it might have emerged.
“The hypothesis would be that this passed through somebody immunosuppressed who therefore had circulation of live mutations over a long period of time,” he said.
Is 501Y more virulent?
“There is no indication at this point of increased infection severity associated with the new variant,” the ECDC said in its threat assessment.
This conclusion, however, “is challenged by the fact that the majority of cases were reported in people under 60 years old, who are less likely to develop severe symptoms.”
At the same time, “there is a hint that it has a higher propensity to infect children,” said Ferguson.
Even if proven true, that does not mean that the virus is “targeting” children, who up to now have been less prone to infection and, when they do catch the bug, severe symptoms, said Barclay.
“The previous virus had a harder time binding to ACE2 and getting into (human) cells,” she explained. That made adults—with more abundant ACE2 receptors in their nose and throats—an easier target compared to children.
“If the new strain is having an easier time of entering and binding to cells, that would put children on a more level playing field,” Barclay added, noting the additional impact of young people mixing socially, especially in school.
Will vaccines still work?
Scientists in Britain and elsewhere are testing the new strain against the several SARS-CoV-2 vaccines, but so far there is no indication that they will be less effective against 501Y.
“It is possible that we may need to update vaccines, perhaps not every year,” said Barclay. “But we will need to monitor these viruses moving forward.”
Updating the new generation of so-called messenger RNA vaccines, she added, will be a lot easier than modifying flu vaccines, as happens every year.
Both of the leading vaccines in Europe and the US—one made by Pfizer-BioNTech, the other by Moderna—are RNA-based.
The co-founder of BioNTech, Ugur Sahin, said Tuesday it was “highly likely” that its vaccine would work against the mutated strain detected in Britain, adding that the company could adapt the vaccine if necessary in six weeks.
Researchers are also investigating the possible impact of the new strain on COVID-19 testing and treatments, though there is little so far to suggest either will be significantly compromised.
Source: Read Full Article
