Lipopolysaccharide, a virulence factor produced by bacteria, is a toxin that can cause a systemic inflammation via the circulation. In a recently completed study, genetic markers were discovered which are associated with a heightened lipopolysaccharide level in the blood.
Microbes are part of the human body, and bacteria or their components often end up in the circulation. One such bacterial component is lipopolysaccharide (LPS), which is a toxin. High concentrations of LPS in the blood cause sepsis. Low LPS levels, known as endotoxemia, cause low-grade inflammation. In fact, endotoxemia commonly occurs in connection with, for example, obesity, predicting a heightened risk for both diabetes and cardiovascular diseases.
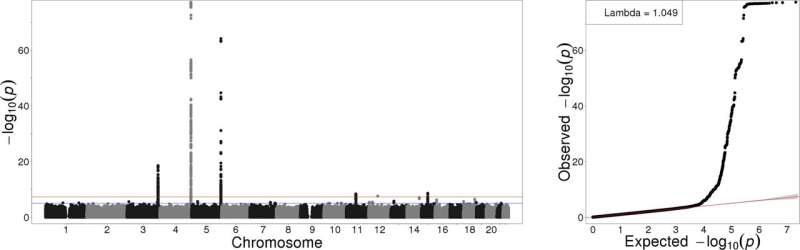
In a study recently completed at the University of Helsinki, LPS levels were measured in the blood of more than 11,000 Finns, after which genome-wide association analyses were carried out to chart the link to the genome. Utilized in further analyses was the FinnGen cohort, which includes genome and disease data on close to 200,000 Finns. The study was carried out collaboratively by the University of Helsinki, the Folkhälsan Research Center, the Finnish Institute for Health and Welfare and the French Institute of Health and Medical Research (INSERM).
“As an entirely new find, we identified an apparent link between the human genome and the amount of bacterial toxins in the blood,” says researcher Jaakko Leskelä.
Low-grade inflammation linked to thrombosis
Blood coagulation and defense against infections are interlinked traits, which is in fact beneficial for, for example, the healing of wounds: bleeding must be arrested, while the wound must be protected against infection. In the recently published study, a link between endotoxemia and certain genes associated with blood coagulation was found.
“Our findings connected endotoxemia particularly with blood clots, strokes and other diseases related to blood coagulation,” Leskelä says.
Consequently, the genes which have such a favorable effect on wound healing also have an unfavorable connection to low-grade inflammation in the body.
“While we do not yet know how exactly these genes associated with coagulation can affect endotoxemia, demonstrating a link is a big step forward as such,” Leskelä notes.
The results also indicate that the quality of the human microbiome makes a difference to the risk of developing cardiovascular diseases.
Source: Read Full Article
