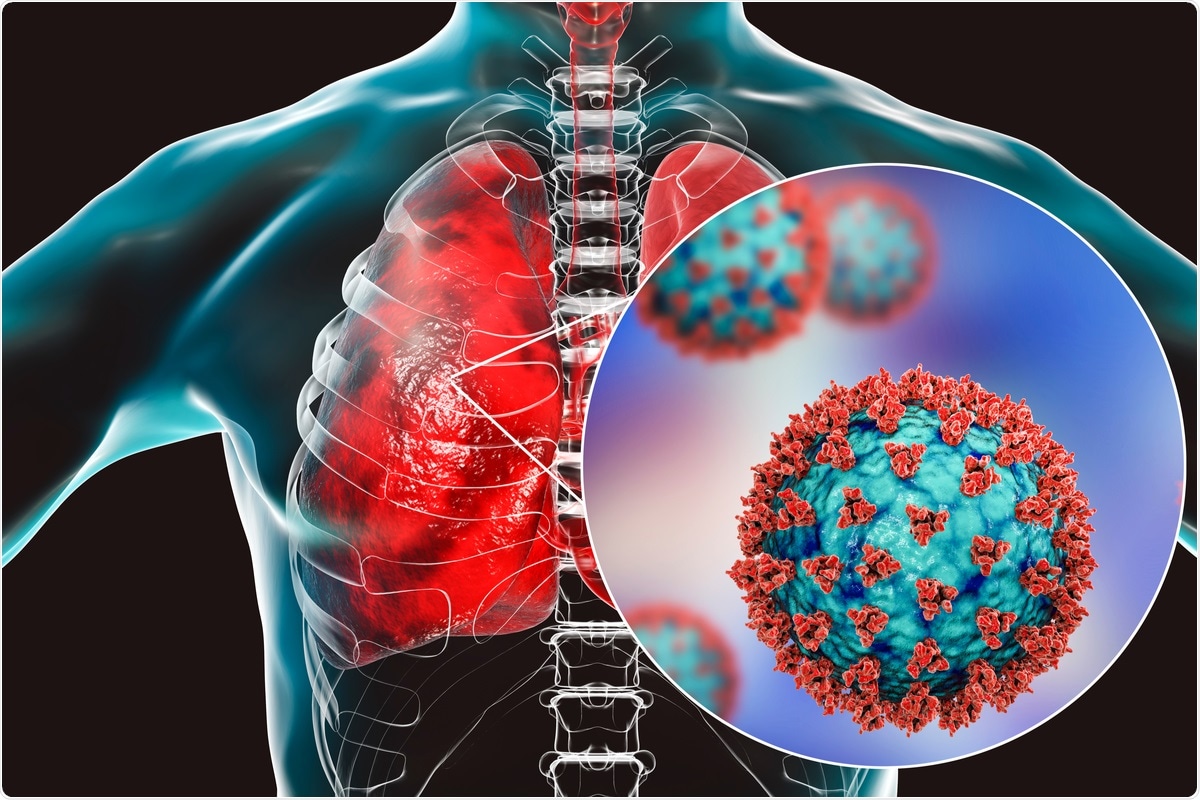
In a recent Thorax state of the art review, researchers discuss the progression of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection throughout the respiratory epithelium. Herein, the authors elaborate on the initial infection stages, pulmonary cell types, innate immune response, and distinct therapeutic strategies from numerous clinical studies, in vivo pathogen-challenged models, and in vitro studies with human respiratory epithelial cells.
Study: Respiratory epithelial cell responses to SARS-CoV-2 in COVID-19. Image Credit: Kateryna Kon / Shutterstock.com
Introduction
SARS-CoV-2 infection, which causes coronavirus disease 2019 (COVID-19), can lead to a range of clinical manifestations from asymptomatic cases to severe disease that can lead to acute respiratory distress syndrome (ARDS) and death in some cases. Even under medical care, COVID-19 patients will have varied responses to treatment, with critically ill patients often unable to improve significantly.
Interestingly, some treatments that are contraindicated in the early stages of COVID-19 have proven to be effective in treating later stages of the disease. In an effort to improve patient outcomes following treatment, it is crucial to understand SARS-CoV-2 pathogenesis in terms of the infection location, the specific cells that are infected, and the stage of infection.
SARS-CoV-2 in the conducting airways
SARS-CoV-2 initially binds its spike (S) protein to the angiotensin-converting enzyme 2 (ACE2) receptor, which is present on the surface of host cells, for its entry. ACE2 is present on the surface of both type I and type II alveolar epithelial cells, as well as various other locations including the nasal and oral mucosa and nasopharynx.
Notably, the expression of ACE2 is highly variable among cells and often found at low levels. In addition to ACE2, the S protein also utilizes the transmembrane serine protease 2 (TMPRSS2) to gain cell entry, which is a serine protease that cleaves the S protein to initiate viral fusion with the cell membrane.
The initial site of SARS-CoV-2 infection is the sinonasal airway epithelium. These cells mediate mucociliary clearance, which is the primary innate defense of the lungs. SARS-CoV-2 infects the ACE2-expressing ciliated cells, replicates, and then infects the neighboring cells upon apical release, which occurs within six hours from the initial infection.
These infected ciliated cells subsequently initiate the innate immune response by secreting interferons and other cytokines. Both the propagation of the virus and activation of the immune system occur nearly simultaneously in infected tissues.
When SARS-CoV-2 succeeds in delaying or dampening the cytokine response, the infected ciliated cells shed their cilia, thus leading to impaired mucociliary clearance. The damaged ciliated and mucous cells leave a denuded epithelial barrier. However, the progenitor-basal cells, which are typically spared from infection, can proliferate and restore the damaged epithelium.
In the next stage, SARS-CoV-2 enters the lower conducting airways, where there are more ciliated cells, mucus-secreting cells, and club cells, all of which express ACE2 and TMPRSS2. This entry stage is highly facilitated for the virus in the geriatric population, as the elderly have diminished cough reflexes and reduced mucociliary clearance.
In these stages of the infection, the innate immune response to SARS-CoV-2 is suppressed or incompletely activated. Only a modest cytokine response, with minimal expression of type I and type III interferons, are observed at this infection stage, which is crucial for cellular and adaptive immune responses. This response in the airways is similar to the modest interferon and cytokine response observed in the nose against SARS-CoV-2.
An early innate immune response is essential for subsequent activation of the adaptive immune response. While immunoglobulin M (IgM), IgG, and IgA are all important for protection against SARS-CoV-2, IgA is crucial for mucosal immunity. To this end, IgA effectively neutralizes SARS-CoV-2 in the first few weeks immediately after the onset of the symptoms.
The reduced innate immune response observed in asymptomatic individuals might cause decreased antibody and T-cell responses. Furthermore, this limited response may prevent the lasting of acquired immunity in these individuals, thereby causing possible breakthrough infections in the future.
Therapeutic strategies for early infection in the upper airways include the use of monoclonal antibodies that have been designed to block virus docking on host ACE2, as well as anti-viral drugs like remdesivir to inhibit subsequent viral replication. However, these treatment options pose challenges, such as the need for an early administration for effectiveness, logistics issues, and possible inactivity against emerging variants.
Inhaled beta interferon to stimulate the innate immune response is another therapeutic agent that is currently being evaluated in Phase II clinical trials. Both systemic and inhaled steroids also remain of interest; however, conclusive results from clinical trials have yet to be achieved.
SARS-CoV-2 in the gas exchange units of lungs
The impact of SARS-CoV-2 in the gas exchange portions of the lung is the primary cause of COVID-19 severity and related mortality. SARS-CoV-2 infection in this region causes progressive hypoxia associated with pulmonary infiltrates, causing alveolar flooding and a robust influx of inflammatory cells.
Rapid progress to ARDS is aided by alveolar damage with loss of functional surfactant, hyaline membranes, epithelial and microvascular injury, and damage to type I and endothelial cells. In some cases, thrombi can form in these vessels and lead to catastrophic events.
In this region, alveolar type II cells express both ACE-2 and TMPRSS2. When SARS-CoV-2 enters the alveoli, it infects the ACE2 expressing alveolar type II cells, which are considered the first responders to initiate anti-viral immunity.
SARS-CoV-2 further propagates to infect bystander type II cells. Induced type I and type III interferons initiate the innate immune response, whereas the inflammatory cytokines and chemokines recruit and activate immune cells. Notably, alveolar type II cells also act as antigen-presenting cells (APC) to initiate T-cell responses at this point in the infection.
Alveolar type II cells are also progenitor cells for alveolar epithelium, which raises concerns for long-term sequelae caused by scaring of these tissues. Overall, the resultant damage in the gas exchange portions of the lungs leads to ARDS.
Some of the therapeutic strategies that have been developed to target alveolar infection are aimed at inhibiting viral replication, preserving type II cell survival and function, and reducing the inflammatory response to maintain the functional integrity of the gas exchange units. Preventing endothelial injury and microvascular thrombi are also crucial at this point in the infection.
Some drugs such as dexamethasone, anti-cytokines (Baricitinib, Tocilizumab, and Sarilumab), corticosteroids, cyclic Cyclic adenosine monophosphate (cyclic AMP), as well as mitogenic growth factors including keratinocyte growth factor (KGF), hepatocyte growth factor (HGF), and transforming growth factor-alpha (TGFa) are used for treating hospitalized COVID-19 patients or testing for the rescue of the alveolar cells. However, the outcomes of these different therapies are highly contextual and considered to be case-dependent.
Severe disease with advanced age
Though the level expression of ACE2 on cells is varied and cell-type independent, its expression in the elderly has been found to be high in alveolar type II cells. When comparing adult and pediatric patients, several studies have reported reduced interferon responses in the epithelial cells and more innate lymphoid and naïve T-cells in the peripheral blood in COVID-19 pediatric patients.
Summary
The treatment outcome of COVID-19 patients depends on the stage of the disease and the type of infected cells. Specifically, the extent of damage to the alveolar epithelium determines mortality and the long-term sequelae of SARS-CoV-2 infection.
Furthermore, damage to the progenitor cells in the conducting airways and the alveoli results in the long-term effects of SARS-CoV-2. While the basal stem cells are spared, type II cell damage is significant.
The current review provides a comprehensive overview of COVID-19 progression in the respiratory epithelium, wherein the authors focus on the distinct cellular characteristics and use of unique therapeutic agents.
- Bridges, J. P., Vladar, E. K., Huang, H., et al. Respiratory epithelial cell responses to SARS-CoV-2 in COVID-19. Thorax. https://thorax.bmj.com/content/77/2/203.
Posted in: Medical Research News | Medical Condition News | Disease/Infection News
Tags: ACE2, Acute Respiratory Distress Syndrome, Adenosine, Angiotensin, Angiotensin-Converting Enzyme 2, Antibodies, Antibody, Antigen, Blood, Cell, Cell Membrane, Chemokines, Cilia, Coronavirus, Coronavirus Disease COVID-19, Cough, covid-19, Cytokine, Cytokines, Dexamethasone, Drugs, Enzyme, Growth Factor, Hypoxia, Immune Response, Immune System, immunity, Immunoglobulin, in vitro, in vivo, Interferon, Interferons, Lungs, Membrane, Mortality, Pathogen, Progenitor Cells, Propagation, Protein, Receptor, Remdesivir, Respiratory, SARS, SARS-CoV-2, Serine, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Stem Cells, Syndrome, T-Cell, Virus

Written by
Dr. Ramya Dwivedi
Ramya has a Ph.D. in Biotechnology from the National Chemical Laboratories (CSIR-NCL), in Pune. Her work consisted of functionalizing nanoparticles with different molecules of biological interest, studying the reaction system and establishing useful applications.
Source: Read Full Article